In what could one day become a new treatment for epilepsy, researchers at UC San Francisco, UC Santa Cruz and UC Berkeley have used pulses of light to prevent seizure-like activity in neurons in brain tissue taken from epilepsy patients as part of their treatment.
Eventually, they hope the technique will replace surgery to remove the brain tissue where seizures originate, providing a less invasive option for patients whose symptoms cannot be controlled with medication.
The team used a method known as optogenetics, which employs a harmless virus to deliver light-sensitive genes from microorganisms to a particular set of neurons in the brain. Those neurons can then be switched on or off with pulses of light.
When the brain is acting normally, neurons send signals at different times and frequencies in a predictable, low-level chatter. But during a seizure, the chatter synchronizes into loud bursts of electrical activity that overwhelm the brain’s casual conversation.
The team used the light pulses to prevent the bursts by switching off neurons that contained light-sensitive proteins.
It is the first demonstration that optogenetics can be used to control seizure-like activity in living human brain tissue, and it opens the door to new treatments for other neurological diseases and conditions.
“This represents a giant step toward a powerful new way of treating epilepsy and likely other conditions,” said Tomasz Nowakowski, PhD, an assistant professor of neurological surgery and a co-senior author of the study, which appears Nov. 15 in Nature Neuroscience.
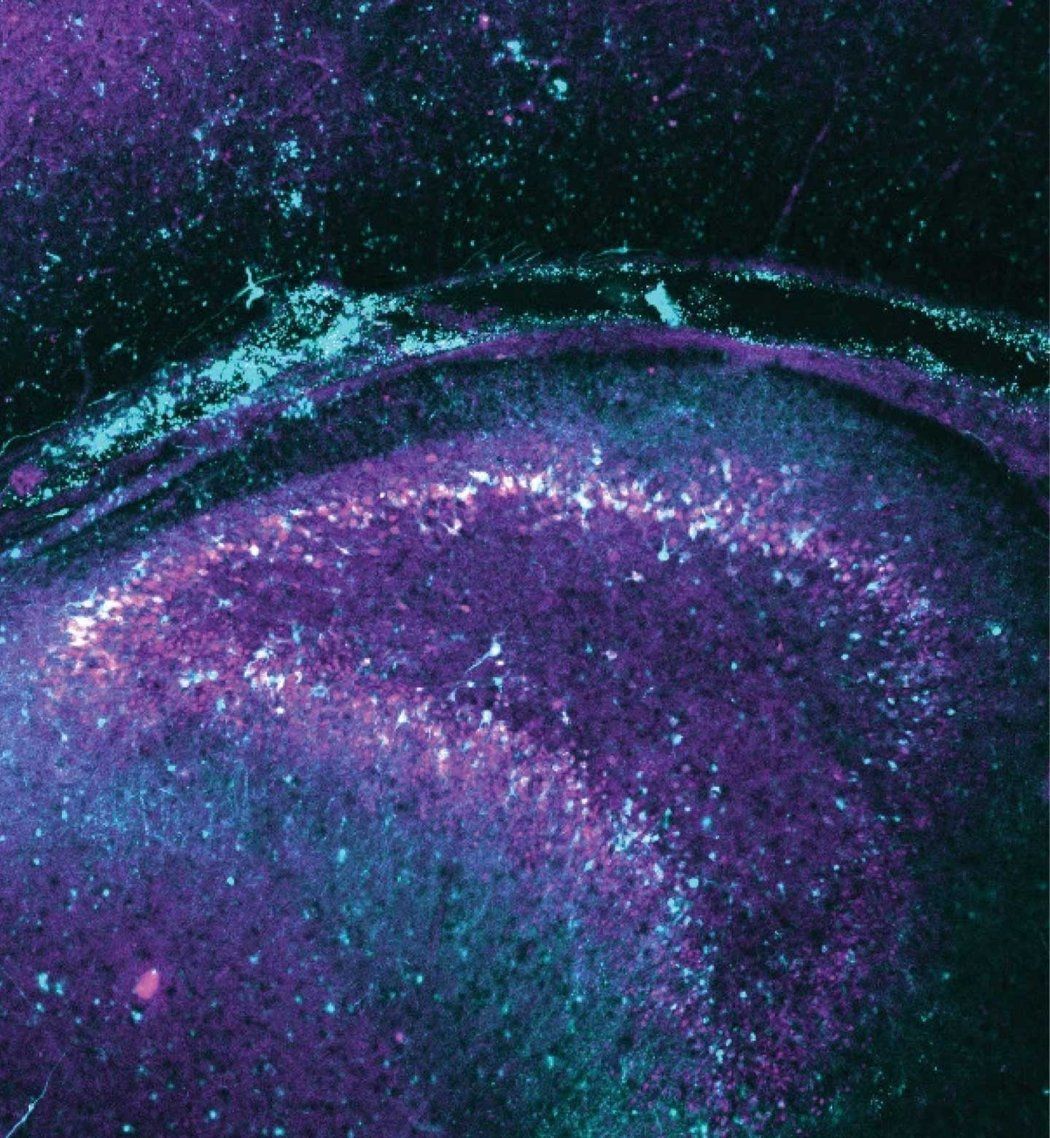
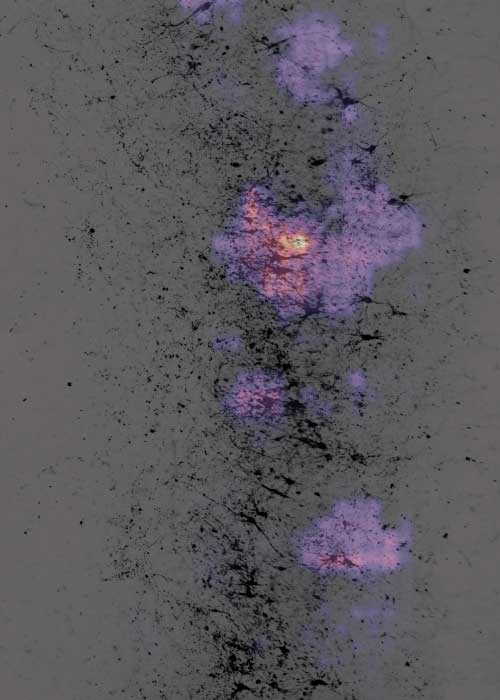
These images show how seizure-like activity can be subdued by pulses of light in a slice of living brain tissue containing light-sensitive proteins.
The pink and yellow reflect seizure-like activity before the light is turned on.
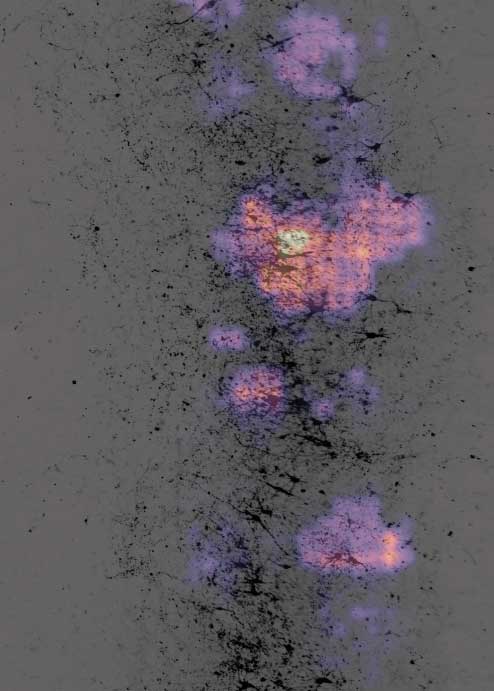
When the cells are illuminated, the abnormal activity dissipates.
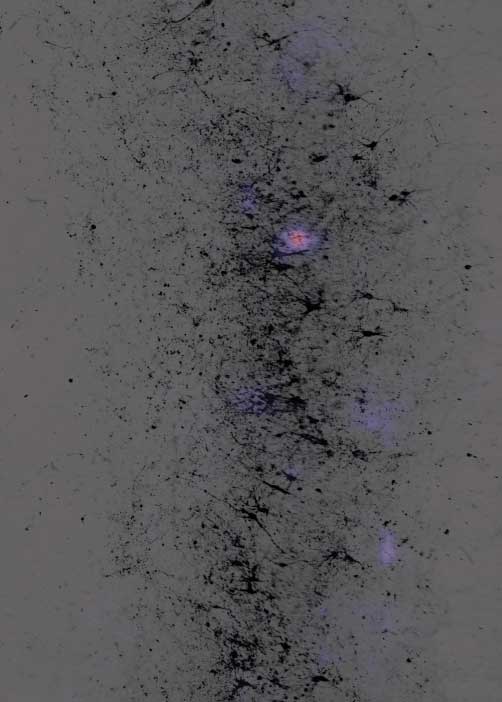
When the light is turned off, abnormal activity starts up again.
Subduing epilepsy’s spikes
To keep the surgically removed tissue alive long enough to complete the study, which took several weeks, the researchers created an environment that mimics conditions inside the skull.
John Andrews, MD, a resident in neurosurgery, placed the tissue on a nutrient medium that resembles the cerebrospinal fluid that bathes the brain.
David Schaffer, PhD, a biomolecular engineer at UC Berkeley found the best virus to deliver the genes, so they would work in the specific neurons the team was targeting.
Andrews then placed the tissue on a bed of electrodes small enough to detect the electrical discharges of neurons communicating with each other.
Scattered dots of blue and red show normal, low-level chatter between neurons. Then, activity synchronizes into solid fields of red and blue, reflecting a seizure. The pattern dissipates when the neurons are illuminated, and returns when the light goes off.
Remote-control experimentation
First, the team needed to find a way to run their experiments without disturbing the tissue. The tiny electrodes were only 17 microns apart – less than half the width of a human hair – and the smallest movement of the brain slices could skew their results.
Mircea Teodorescu, PhD, an associate professor of electrical and computer engineering at UCSC and co-senior author of the study, designed a remote-control system to record the neurons’ electrical activity and deliver light pulses to the tissue.
Teodorescu’s lab wrote software that enabled the scientists to control the apparatus, so the group could direct experiments from Santa Cruz on the tissue in Nowakowski’s San Francisco lab.
That way, no one needed to be in the room where the tissue was being kept.
“This was a very unique collaboration to solve an incredibly complex research problem,” Teodorescu said. “The fact that we actually accomplished this feat shows how much farther we can reach when we bring the strengths of our institutions together.”
New insight into seizures
We’ll be able to give people much more subtle, effective control over their seizures while saving them from such an invasive surgery.”
The technology allowed the team to see that they could stop the seizure-like activity by stimulating a surprisingly small number of neurons as well as determine the lowest intensity of light needed to change the electrical activity.
They were also able to observe how neurons interact while inhibiting a seizure.
These insights provide a deeper understanding of how the approach might be used to tightly regulate brain activity that leads to seizures and could spare patients the invasiveness and side effects of having brain tissue removed, said Edward Chang, MD, the chair of Neurological Surgery at UCSF.
“This kind of approach could really improve care for people with epilepsy,” said Chang, who, along with Nowakowski, is a member of the UCSF Weill Institute for Neurosciences. “We’ll be able to give people much more subtle, effective control over their seizures while saving them from such an invasive surgery.”
Authors: Additional authors on the study: David Shinn, Albert Wang, Matthew Keefe, PhD, Kevin Donohue, Hanh Larson, Kurtis Auguste, MD, Vikaas Sohal, MD, PhD, and Cathryn Cadwell, MD, PhD, of UCSF, Jinghui Geng, Kateryna Voitiuk, Matthew Elliott, Ash Robbins, Alex Spaeth, Daniel Solis, Jessica Sevetson, PhD, Drew Ehrlich, Sofie Salama, PhD, Tal Sharf, PhD, and David Haussler, PhD, of UCSC, and Lin Li and Julio Rivera-de Jesus of UC Berkeley.
Funding: This research was supported by the National Institutes of Health (grants 5R25NS070680-13, UF1MH130700, R01NS123263, R01MH120295, T32HG012344, K08NS126573, K12GM139185 and LRP0000018281), the National Science Foundation (grants 2034037, CNS-1730158, ACI-1540112, ACI-1541349 and OAC-1826967), the Schmidt Futures Foundation (SF 857), Weill Neurohub grant U01NS132353, the Esther A & Joseph Klingenstein Fund, the Shurl and Kay Curci Foundation, the Sontag Foundation, and a gift from the William K. Bowes Jr Foundation.