A genomic test developed at UC San Francisco to rapidly detect almost any kind of pathogen – virus, bacteria, fungus or parasite – has proved successful after a decade of use.
The test has the potential to vastly improve care for neurological infections that cause diseases like meningitis and encephalitis, as well as speed up the detection of new viral pandemic threats, including bird flu and COVID-19. It uses a powerful genomic sequencing technique, called metagenomic next-generation sequencing (mNGS).
Rather than looking for one type of pathogen at a time, mNGS analyzes all the nucleic acids, RNA and DNA, that are present in a sample.
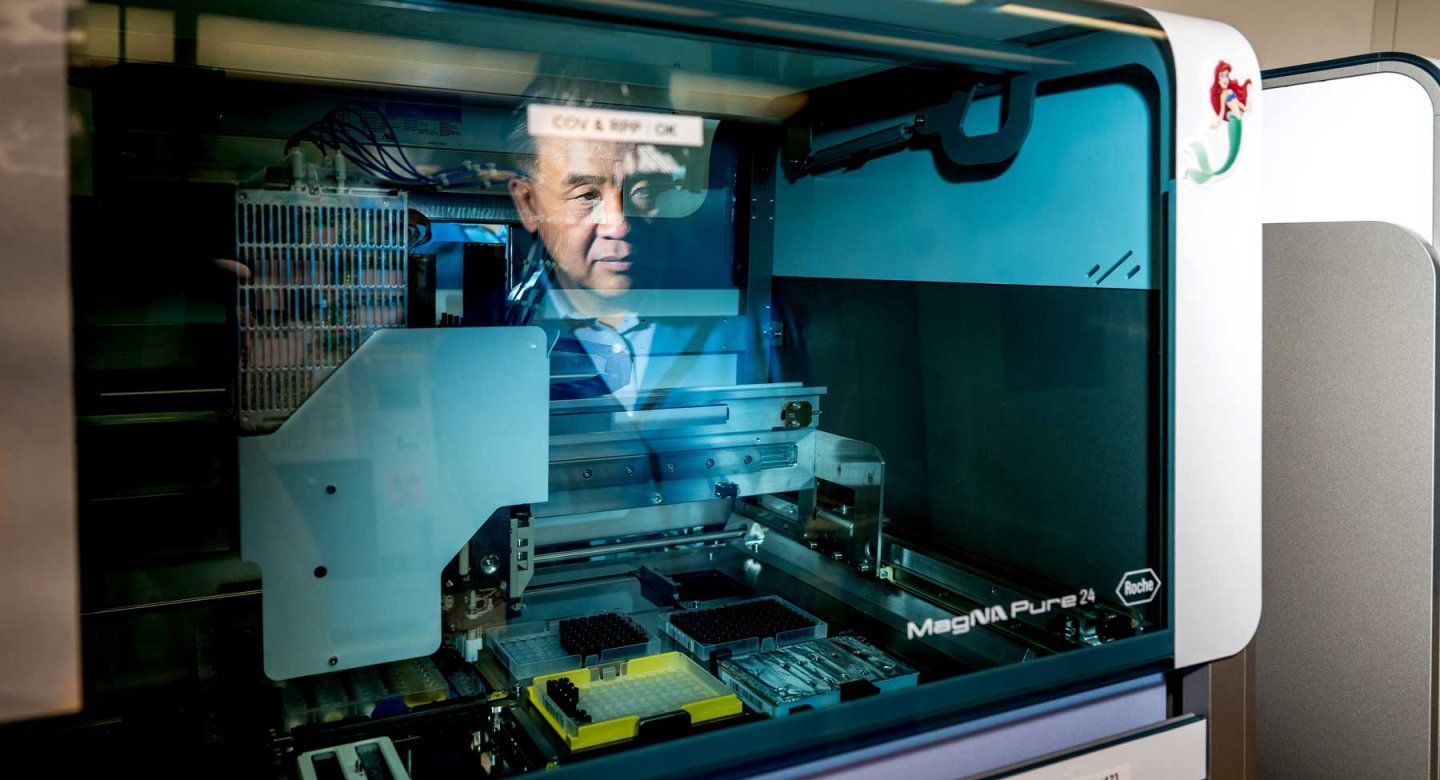
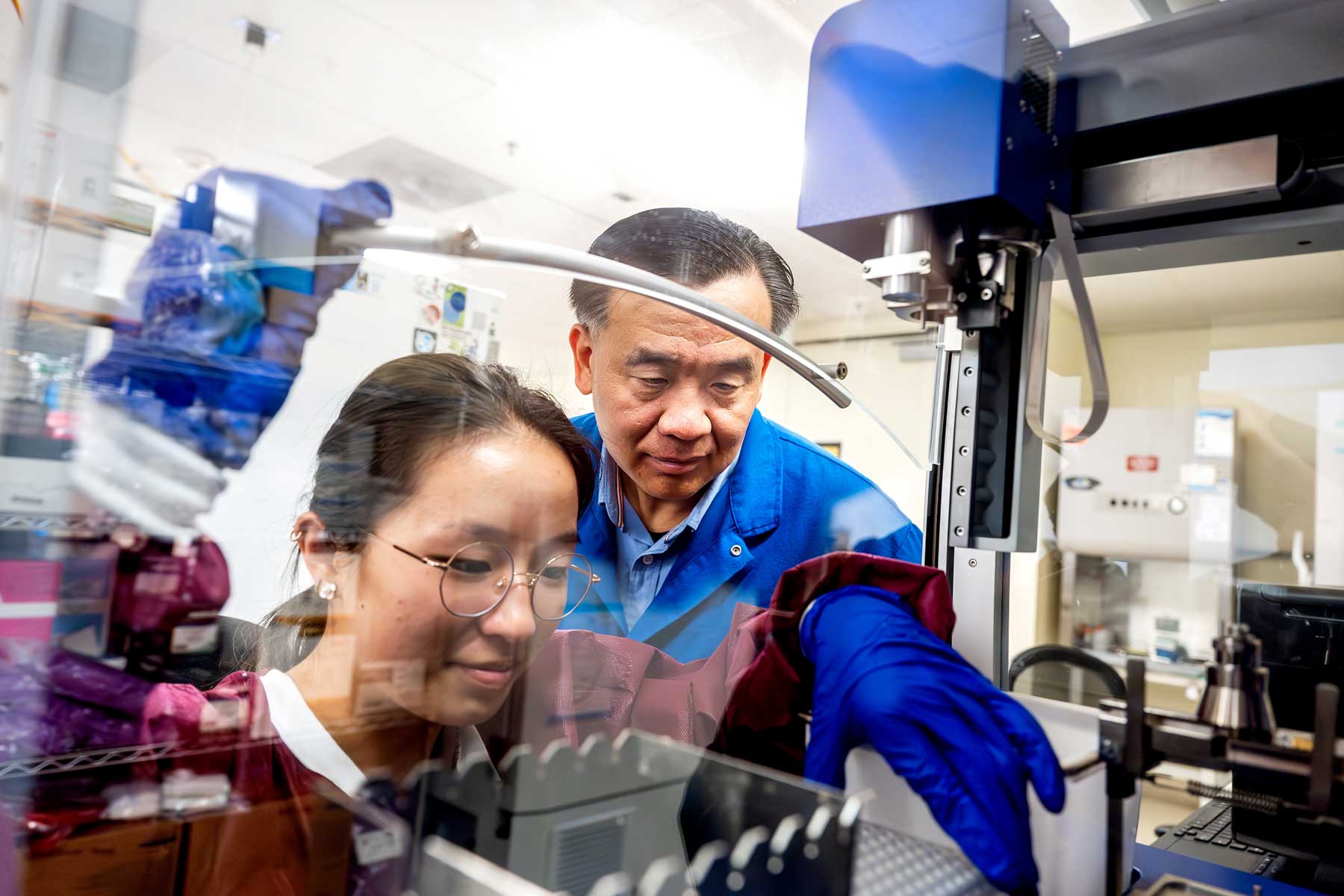
“Our technology is deceptively simple,” said Charles Chiu, MD, PhD, professor of laboratory medicine and infectious diseases at UCSF and senior author of the study. “By replacing multiple tests with a single test, we can take the lengthy guesswork out of diagnosing and treating infections.”
The researchers originally developed a clinical mNGS test to analyze cerebrospinal fluid (CSF), the pristine liquid that bathes the brain and spinal cord.
The test has now been performed on thousands of patients with unexplained neurological symptoms, both at UCSF and other hospitals across the country.
In a paper that appears Nov. 12 in Nature Medicine, the team demonstrated that the mNGS test correctly identified 86% of neurological infections.
In a companion study published the same day in Nature Communications, the team also used mNGS to identify pathogens in respiratory fluid that can cause pneumonia, and automated it to get results faster.
They expect that the automated test will be able to detect novel viral pathogens that could cause respiratory pandemics like COVID-19.
The types of infections that can threaten our brains and lungs
Different types of pathogens – bacterial, fungal, parasitic or viral – can invade our bodies and cause life-threatening diseases, especially when they can’t be quickly diagnosed and properly treated. The mNGS test developed at UCSF correctly identified 86% of neurological infections, some of which are caused by the types of pathogens below.
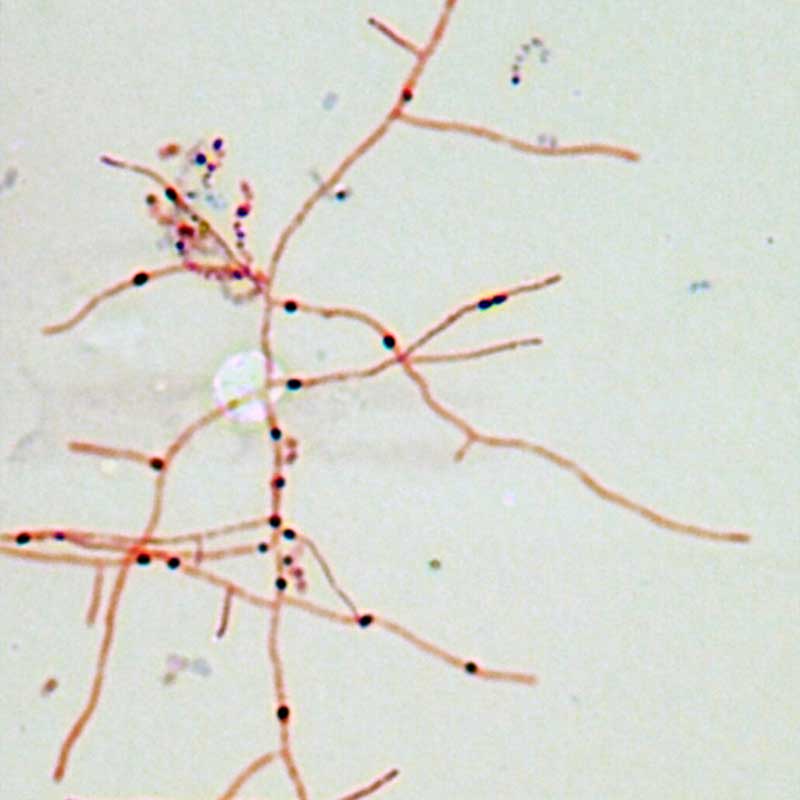
Bacterial
Bacteria like Nocardia, as seen above, can cause pneumonia or encephalitis. Image by Chiu Lab
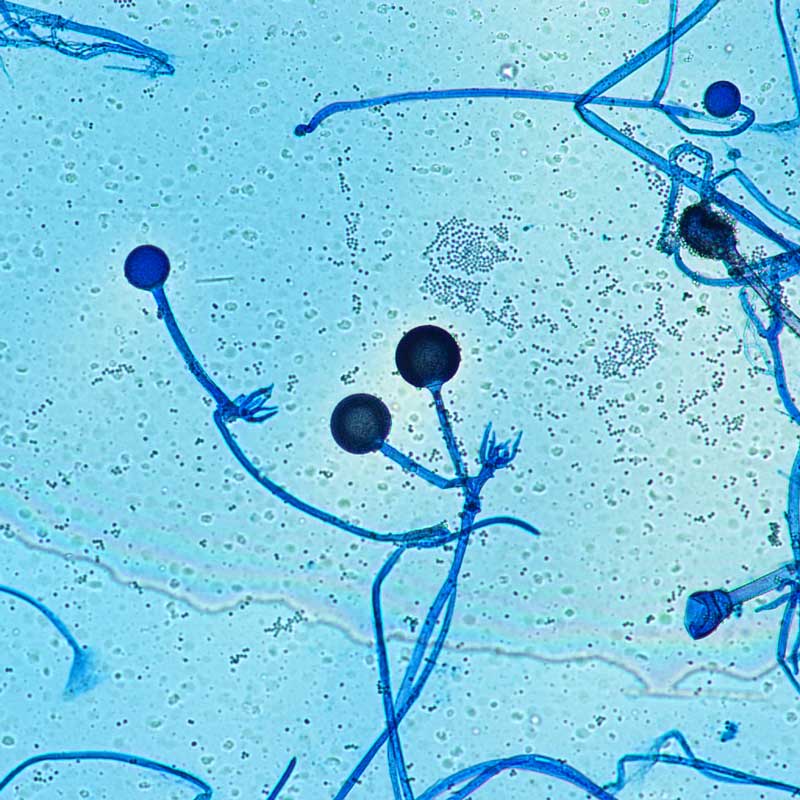
Fungal
Fungi such as Rhizopus, pictured above, can infect cerebrospinal fluid and respiratory fluid. Image by Chiu Lab
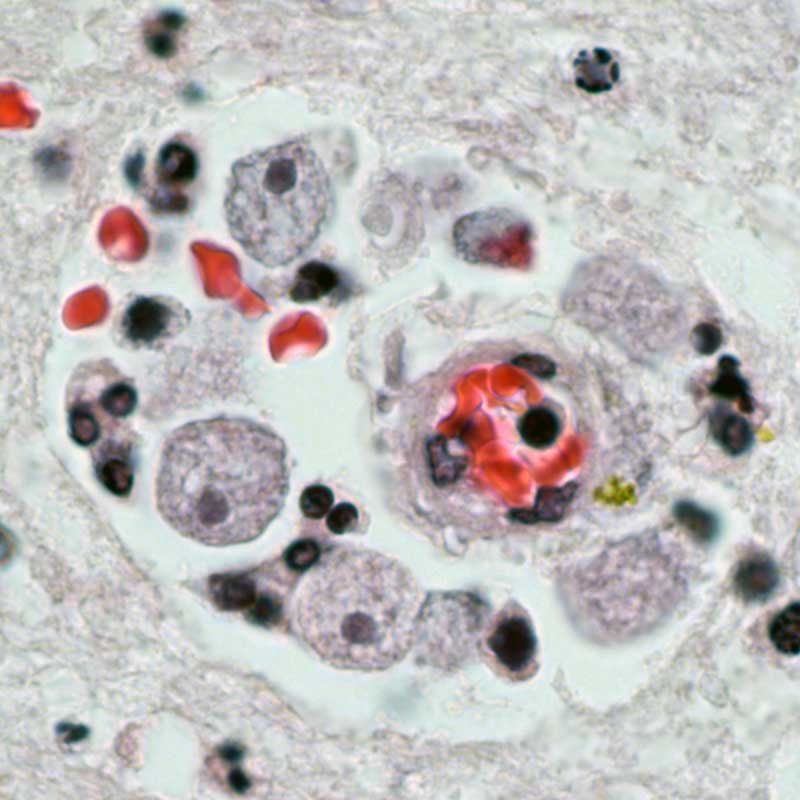
Parasitic
Here, Acanthamoeba parasites, known as the “brain eating amoeba”, carved a hole in the brain and are also ingesting red blood cells. Image by Chiu Lab
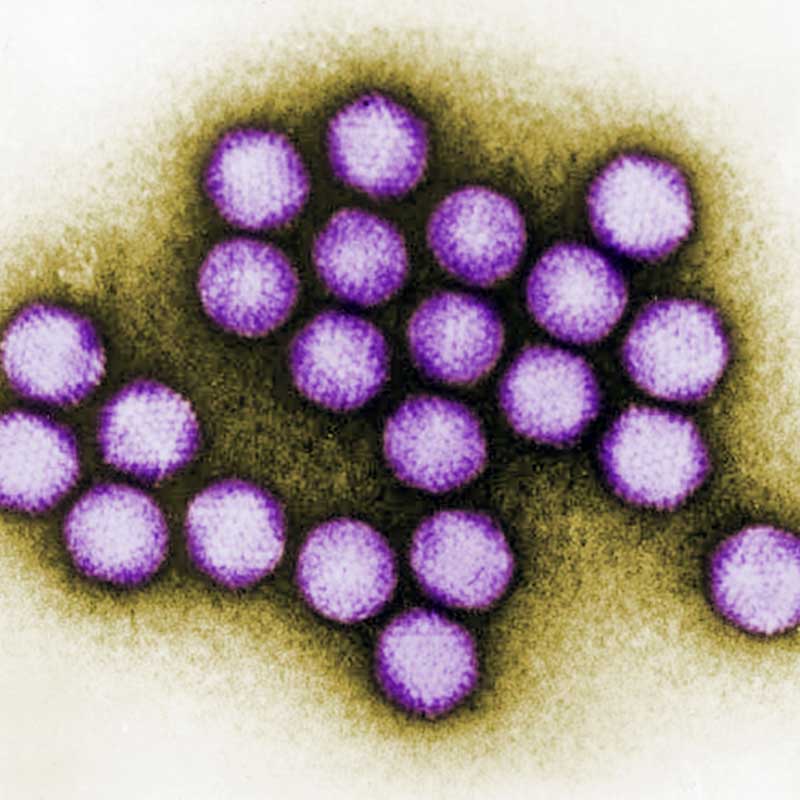
Viral
Adenoviruses in cerebrospinal fluid and respiratory fluid can cause diseases like bronchitis or pneumonia. Image by Centers for Disease Control
A breakthrough in diagnosing rare, infectious neurological disease
Neurological diseases can be very hard to diagnose, especially when the cause is a rare or previously unknown pathogen. In many cases, each day without a diagnosis means a continual worsening of a patient’s condition.
In the early 2010s, Chiu, along with UCSF colleagues Joe DeRisi, PhD, and Michael Wilson, MD, developed a novel metagenomic sequencing method to test CSF for potential pathogens causing neurologic infections.
The test works by sequencing all the genetic material in CSF, then running a computational analysis pipeline to separate human sequences from those that originate from bacteria, viruses, fungi or parasites.
In 2014, the team used the technology to help doctors in Wisconsin treat a young boy who was critically ill in the intensive care unit with an undiagnosed infection.
A long series of tests had failed to find out what was wrong with him, but UCSF’s test took just 48 hours to reveal that the boy had leptospirosis, which is treatable with penicillin. His doctors gave it to him, and he fully recovered.
Our mNGS test performs better than any other category of test for neurologic infections.”
The mNGS test soon became routine at UCSF, with hospitals and clinics nationwide sending samples to be processed by the UCSF Clinical Microbiology Laboratory, of which Chiu is the director.
Between 2016 and 2023, the UCSF team analyzed nearly 5,000 CSF samples with the test, 14.4% of which turned out to have an infection. In those samples, the test accurately identified the pathogen 86% of the time.
“Our mNGS test performs better than any other category of test for neurologic infections,” Chiu said, “The results support its use as a critical part of the diagnostic armamentarium for physicians who are working up patients with infectious diseases.”
To increase access to this technology, Chiu, DeRisi, Wilson and others helped found Delve Bio, which is now the exclusive provider of the mNGS CSF test developed at UCSF.
“These findings support including mNGS as a core tool in the clinical workup for CNS infections,” said Steve Miller, MD, PhD, chief medical officer of Delve Bio. “mNGS offers the single most unbiased, complete and definitive tool for pathogen detection. Thanks to its ability to quickly diagnose an infection, mNGS helps guide management decisions and treatment for patients with meningitis and encephalitis, potentially reducing healthcare costs down the line.”
Preparing for the next pandemic
If it is going to serve as an early-warning system for pandemics, the mNGS test must be fast. Chiu and his colleagues have adapted it to work with respiratory fluid and figured out how to automate it.
Whereas the CSF test entails more than 100 separate steps and can take 2 to 7 days to process, the respiratory test requires just 30 minutes of hands-on time before robots and algorithms can take over.
“Our goal was to have the entire process completed within 12 to 24 hours, giving a same-day or next-day result,” Chiu said.
In the Nature Communications study, the researchers demonstrated that the test could detect respiratory viruses with pandemic potential, including SARS-CoV-2, influenza A and B, and RSV in less than a day, even when there were only small amounts of virus present in a sample.
They also modeled the technology’s ability to detect divergent viruses – or newly-evolved strains – and found that it could hypothetically detect all of them, should they emerge in the future.
Both the CSF and respiratory versions of the mNGS test have received breakthrough device designation from the U.S. Food and Drug Administration (FDA).
Authors: For the Nature Medicine paper, other UCSF authors are Patrick Benoit, MD, Noah Brazer, Mikael de Lorenzi-Tognon, MD, PhD, Emily Kelly, MD, MS, Venice Servellita, MS, Miriam Oseguera, Jenny Nguyen, MD, MA, Jack Tang, MHS, Charles Omura, Jessica Streithorst, PhD, Melissa Hillberg, Danielle Ingebrigtsen, MHS, Kelsey Zorn, MHS, and Michael R. Wilson, MD. For all authors, see the paper.
For the Nature Communications paper, other UCSF authors are Jessica Karielle Tan, PhD, Venice Servellita, MS, Doug Stryke, Emily Kelly, MD, MS, Jessica Streithorst, PhD, Nanami Sumimoto, Abiodun Foresythe, Hee Jae Huh, Jenny Nguyen MD, MA, Miriam Oseguera, Noah Brazer, Jack Tang, MHS, Danielle Ingebrigtsen, MHS, Becky Fung, Helen Reyes, Melissa Hillberg, Peter M. Mourani, Charles R. Langelier, MD, PhD, Mikael de Lorenzi-Tognon, MD, PhD, and Patrick Benoit, MD. For all authors, see the paper.
Funding: The Nature Medicine paper was supported in part by a BARDA EZ-BAA award 75A50122C00022, US CDC grants 75D30122C15360 and 75D30121C12641 and the Chan Zuckerberg Biohub San Francisco.
The Nature Communications paper was supported in part by in part by a BARDA EZ-BAA 494 award 75A50122C00022, US CDC grants 75D30122C15360 and 75D30121C12641, Abbott Laboratories and the Chan Zuckerberg Biohub San Francisco.
Disclosures: Chiu is a founder of Delve Bio and serves on its scientific advisory board, as well as those of Flightpath Biosciences, Biomeme, Mammoth Biosciences, BiomeSense and Poppy Health. He is also an inventor on US patent 509 11380421, “Pathogen detection using next generation sequencing.” Wilson is a co-founder and serves on the scientific advisory board and board of directors for Delve Bio.
A breakthrough in diagnosing rare, infectious neurological disease
Neurological diseases can be very hard to diagnose, especially when the cause is a rare or previously unknown pathogen. In many cases, each day without a diagnosis means a continual worsening of a patient’s condition.
In the early 2010s, Chiu, along with UCSF colleagues Joe DeRisi, PhD, and Michael Wilson, MD, developed a novel metagenomic sequencing method to test CSF for potential pathogens causing neurologic infections.
The test works by sequencing all the genetic material in CSF, then running a computational analysis pipeline to separate human sequences from those that originate from bacteria, viruses, fungi or parasites.
In 2014, the team used the technology to help doctors in Wisconsin treat a young boy who was critically ill in the intensive care unit with an undiagnosed infection.
A long series of tests had failed to find out what was wrong with him, but UCSF’s test took just 48 hours to reveal that the boy had leptospirosis, which is treatable with penicillin. His doctors gave it to him, and he fully recovered.
Our mNGS test performs better than any other category of test for neurologic infections.”
The mNGS test soon became routine at UCSF, with hospitals and clinics nationwide sending samples to be processed by the UCSF Clinical Microbiology Laboratory, of which Chiu is the director.
Between 2016 and 2023, the UCSF team analyzed nearly 5,000 CSF samples with the test, 14.4% of which turned out to have an infection. In those samples, the test accurately identified the pathogen 86% of the time.
“Our mNGS test performs better than any other category of test for neurologic infections,” Chiu said, “The results support its use as a critical part of the diagnostic armamentarium for physicians who are working up patients with infectious diseases.”
To increase access to this technology, Chiu, DeRisi, Wilson and others helped found Delve Bio, which is now the exclusive provider of the mNGS CSF test developed at UCSF.
“These findings support including mNGS as a core tool in the clinical workup for CNS infections,” said Steve Miller, MD, PhD, chief medical officer of Delve Bio. “mNGS offers the single most unbiased, complete and definitive tool for pathogen detection. Thanks to its ability to quickly diagnose an infection, mNGS helps guide management decisions and treatment for patients with meningitis and encephalitis, potentially reducing healthcare costs down the line.”
Preparing for the next pandemic
If it is going to serve as an early-warning system for pandemics, the mNGS test must be fast. Chiu and his colleagues have adapted it to work with respiratory fluid and figured out how to automate it.
Whereas the CSF test entails more than 100 separate steps and can take 2 to 7 days to process, the respiratory test requires just 30 minutes of hands-on time before robots and algorithms can take over.
“Our goal was to have the entire process completed within 12 to 24 hours, giving a same-day or next-day result,” Chiu said.
In the Nature Communications study, the researchers demonstrated that the test could detect respiratory viruses with pandemic potential, including SARS-CoV-2, influenza A and B, and RSV in less than a day, even when there were only small amounts of virus present in a sample.
They also modeled the technology’s ability to detect divergent viruses – or newly-evolved strains – and found that it could hypothetically detect all of them, should they emerge in the future.
Both the CSF and respiratory versions of the mNGS test have received breakthrough device designation from the U.S. Food and Drug Administration (FDA).
Authors: For the Nature Medicine paper, other UCSF authors are Patrick Benoit, MD, Noah Brazer, Mikael de Lorenzi-Tognon, MD, PhD, Emily Kelly, MD, MS, Venice Servellita, MS, Miriam Oseguera, Jenny Nguyen, MD, MA, Jack Tang, MHS, Charles Omura, Jessica Streithorst, PhD, Melissa Hillberg, Danielle Ingebrigtsen, MHS, Kelsey Zorn, MHS, and Michael R. Wilson, MD. For all authors, see the paper.
For the Nature Communications paper, other UCSF authors are Jessica Karielle Tan, PhD, Venice Servellita, MS, Doug Stryke, Emily Kelly, MD, MS, Jessica Streithorst, PhD, Nanami Sumimoto, Abiodun Foresythe, Hee Jae Huh, Jenny Nguyen MD, MA, Miriam Oseguera, Noah Brazer, Jack Tang, MHS, Danielle Ingebrigtsen, MHS, Becky Fung, Helen Reyes, Melissa Hillberg, Peter M. Mourani, Charles R. Langelier, MD, PhD, Mikael de Lorenzi-Tognon, MD, PhD, and Patrick Benoit, MD. For all authors, see the paper.
Funding: The Nature Medicine paper was supported in part by a BARDA EZ-BAA award 75A50122C00022, US CDC grants 75D30122C15360 and 75D30121C12641 and the Chan Zuckerberg Biohub San Francisco.
The Nature Communications paper was supported in part by in part by a BARDA EZ-BAA 494 award 75A50122C00022, US CDC grants 75D30122C15360 and 75D30121C12641, Abbott Laboratories and the Chan Zuckerberg Biohub San Francisco.
Disclosures: Chiu is a founder of Delve Bio and serves on its scientific advisory board, as well as those of Flightpath Biosciences, Biomeme, Mammoth Biosciences, BiomeSense and Poppy Health. He is also an inventor on US patent 509 11380421, “Pathogen detection using next generation sequencing.” Wilson is a co-founder and serves on the scientific advisory board and board of directors for Delve Bio.