This Global Health Initiative Improves Patient Care in 13 Countries
UCSF fellows receive training, mentoring and funding for research and care. It’s all part of a plan to build the next generation of frontline providers from Burundi to San Francisco.
It had been a day for the record books.
Earlier in his shift at Kibuye Hope Hospital in rural Burundi, Alliance Niyukuri, MD, and his team saved the life of a newborn baby boy with gastroschisis, a birth defect that causes a baby’s intestines to grow outside of its abdomen. No newborn in rural Burundi had ever survived more than a day with the condition, and Niyukuri had treated the tiny baby with a medical device that made it possible for him to survive his first 24 hours and have a hopeful prognosis for his future. Niyukuri was eager to share the momentous news, so he texted his colleagues who helped make it possible – 9,500 miles away in San Francisco.
Niyukuri is the first pediatric surgeon in Burundi, the small landlocked country in East Africa that’s considered one of the poorest in the world. He’s also a fellow with UCSF’s Center for Health Equity in Surgery and Anesthesia (CHESA), which is how he connected with mentors and colleagues who helped make that lifesaving moment possible.
In many low-income countries, people are disabled by or die of things they don’t die of in higher income countries.
Since it started in 2020, CHESA has used research, education and advocacy to improve access to safe surgical, anesthetic and perioperative care in underserved areas of the U.S. and globally, as well as build a pipeline of care providers from diverse backgrounds. It is one of eight core centers in the UCSF Institute for Global Health Sciences. CHESA also co-leads the UCSF-World Health Organization (WHO) Collaborating Centre for Emergency, Critical and Operative Care (ECO) with the UCSF Department of Emergency Medicine, providing medical and technical expertise and support for WHO ECO care projects.
In 2021, CHESA launched a multidisciplinary fellowship for physicians, nurses and advanced practice providers from medical institutions around the world who demonstrate their commitment to health equity in perioperative care, including Niyukuri. During the 18-month fellowship, fellows learn about global health equity, gain access to UCSF educational resources, and receive UCSF faculty mentorship and catalytic funding for research projects. They join a highly diverse and global learning community of fellows, alumni and CHESA faculty who support their growth and professional development.
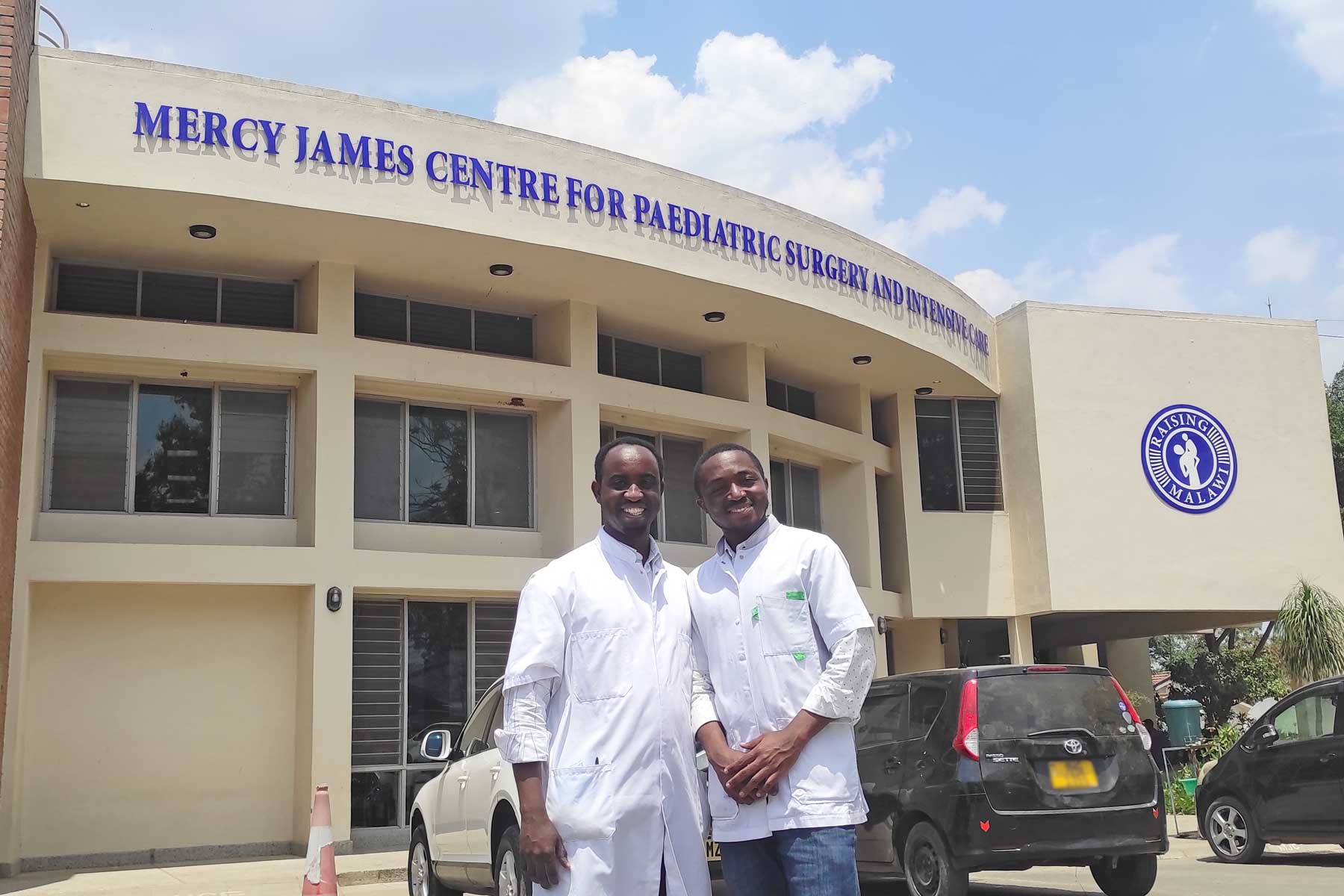
CHESA’s 56 fellows and alumni reach across 14 medical specialties and 13 countries, including Ethiopia, Haiti, Malawi, Romania, Uganda and the U.S. Sixty-five percent of CHESA fellows are from low- and middle-income countries, and 96% are practicing clinicians or frontline providers who serve vulnerable populations worldwide.
Over 5 billion people lack access to safe surgical and anesthetic care when they need it, and global surgery and anesthesia remain critically underfunded and overlooked, explained Doruk Ozgediz, MD, director of UCSF’s Center for Global Surgery and Health Equity and a CHESA co-founder.
“Equity challenges and health disparities are unacceptable, and they know no geographic boundary,” he said. “If you’re in the Bay Area, living two miles apart can mean a 20-year life expectancy difference. In many low-income countries, people are disabled by or die of things they don’t die of in higher-income countries. We created CHESA to improve access to care for vulnerable patients by building the capacity of clinicians who are leading their communities in overcoming their most pressing challenges.”
“CHESA’s multidisciplinary group approach is at the foundation of its success,” said Ozgediz, who started working in Uganda more than 20 years ago when he was a resident at UCSF. “We found that where one person has a challenge, someone else in the CHESA community – either in their country or another one – has a solution since they’ve encountered it. A cross-pollination of ideas and solutions happens naturally, and we learn a lot from each other, especially how to do more with less.”

Best way to spread the word about better outcomes
“Before me, there were no pediatric surgeons in Burundi. Children were dying or suffering from treatable conditions because we didn’t have the specialty training available, especially in our rural areas,” said Niyukuri, who was born in rural Burundi but spent 12 years growing up as a refugee in Kenya, ultimately returning to Burundi for medical school and now practicing medicine there.
“The CHESA fellowship helped me figure out how to start the first pediatric surgery program in Burundi,” he said. “I made important connections with CHESA alumni, faculty and partners who are also African doctors, in Uganda in particular, who had started similar programs in their countries, and I was able to learn from them.”

Niyukuri’s interactions with UCSF faculty and residents helped him make great strides. “Doruk and I talked a lot about how to determine what we needed in Burundi. And I didn’t have a lot of experience designing research, so Caroline [Stephens, MD] was very helpful in the technical design aspect of my research,” he said. “But we have an equitable collaboration, we don’t feel the difference between high-income or low-income, U.S. or Africa.”
It was actually Stephens, a surgical resident at UCSF, who Niyukuri texted when he saved the life of the newborn with the intestinal birth defect. While working together on his research project, he and Stephens talked about other challenges they each faced. She was able to secure the donation of the medical device that Niyukuri used to put the baby’s intestines back into her body.
“It’s a huge milestone that Alliance’s patient survived,” said Stephens, a CHESA fellowship alumnus who has worked on pediatric surgery projects in Uganda and Ethiopia. “Too often people in low- and moderate-income countries are told their problems are not fixable, but that’s not necessarily true with the right resources and training. The best way to spread the word that better outcomes are possible is to show successes like Alliance’s patient, and to prove that specialty surgery is an important resource to have in your country.”
Mistrust of medical providers among some patients
During her fellowship in global health equity in anesthesia at UCSF, Betelehem Asnake, MS, MD, was able to address health disparities she witnessed throughout her medical training. For example, a lot of her Hispanic patients were less likely to get epidurals for fear of being paralyzed, leading to poor pain management and a higher likelihood of general anesthesia if they needed a cesarean section. She witnessed Black patients getting less pain medication after surgeries, and non-native English speaking patients not getting the same care as native speakers.
This inspired Asnake to use her CHESA fellowship to create UCSF’s first health equity curriculum for anesthesia residents. “We take care of patients every day, we should all be aware of health disparities,” she said. “With the health equity curriculum, we talk a lot about why there is a mistrust of medical providers in many minority patients and how to mitigate that. We give anesthesia residents tools and ideas to minimize health inequity in the care our patients receive.”
We must fundamentally change the current reality that anyone may live, die or be disabled simply due to where in the world they happen to be born, the neighborhood they live in, the color of their skin or their personal or family circumstances.”
Doruk Ozgediz, MDDirector of UCSF’s Center for Global Surgery and Health Equity and CHESA co-founder
The curriculum includes a series of interactive lectures and workshops on social determinants of health, cultural humility and competency, structural inequities in the medical system and safety net systems like insurance and Medicare.
Asnake joined UCLA two years ago, bringing UCSF’s health equity curriculum to that program. She’s now in conversation with Stanford University, UC Davis and other schools that want to hear more and possibly implement her health equity curriculum there.
“The CHESA fellowship gave me a rare flexibility and freedom during my fellowship to create this health equity curriculum, and now we’re bringing it to other schools,” said Asnake. “My mentor, Michael Lipnick, MD, let me expand my wings in the directions I wanted to, and now I let my residents do the same. As a result, more residents are learning about health disparities and incorporating what they learn into how they treat their patients.”
Health equity is the most pressing challenge of our generation, said Ozgediz. “We must fundamentally change the current reality that anyone may live, die or be disabled simply due to where in the world they happen to be born, the neighborhood they live in, the color of their skin or their personal or family circumstances.”
“The CHESA fellowship nurtures and develops future leaders who are not only addressing immediate clinical challenges but also these social determinants of health,” he said. “CHESA got its start as the culmination of decades of health equity and global health work across multiple UCSF departments and programs. Now, we’re growing pivotal programs in the surgery and perioperative spaces to tackle health disparities, expand our partnerships, and advocate for our most vulnerable communities, whether they’re in our own backyard or beyond our borders.”