The World Health Organization last week declared mpox (previously monkeypox) to be a global health emergency. The disease experienced a global outbreak in 2022, which subsided in Europe, Asia and the Americas but continued to increase in parts of Africa. New cases in Burundi, Kenya, Uganda, Rwanda and, most recently, a case in Sweden, prompted the WHO’s declaration of mpox as a Public Health Emergency of International Concern or global health emergency.
Seth Blumberg, MD, Ph.D., assistant professor at UC San Francisco, who studied the spread of mpox in the Democratic Republic of the Congo in 2011, explains the viral disease and what the declaration means for us.
What is mpox?
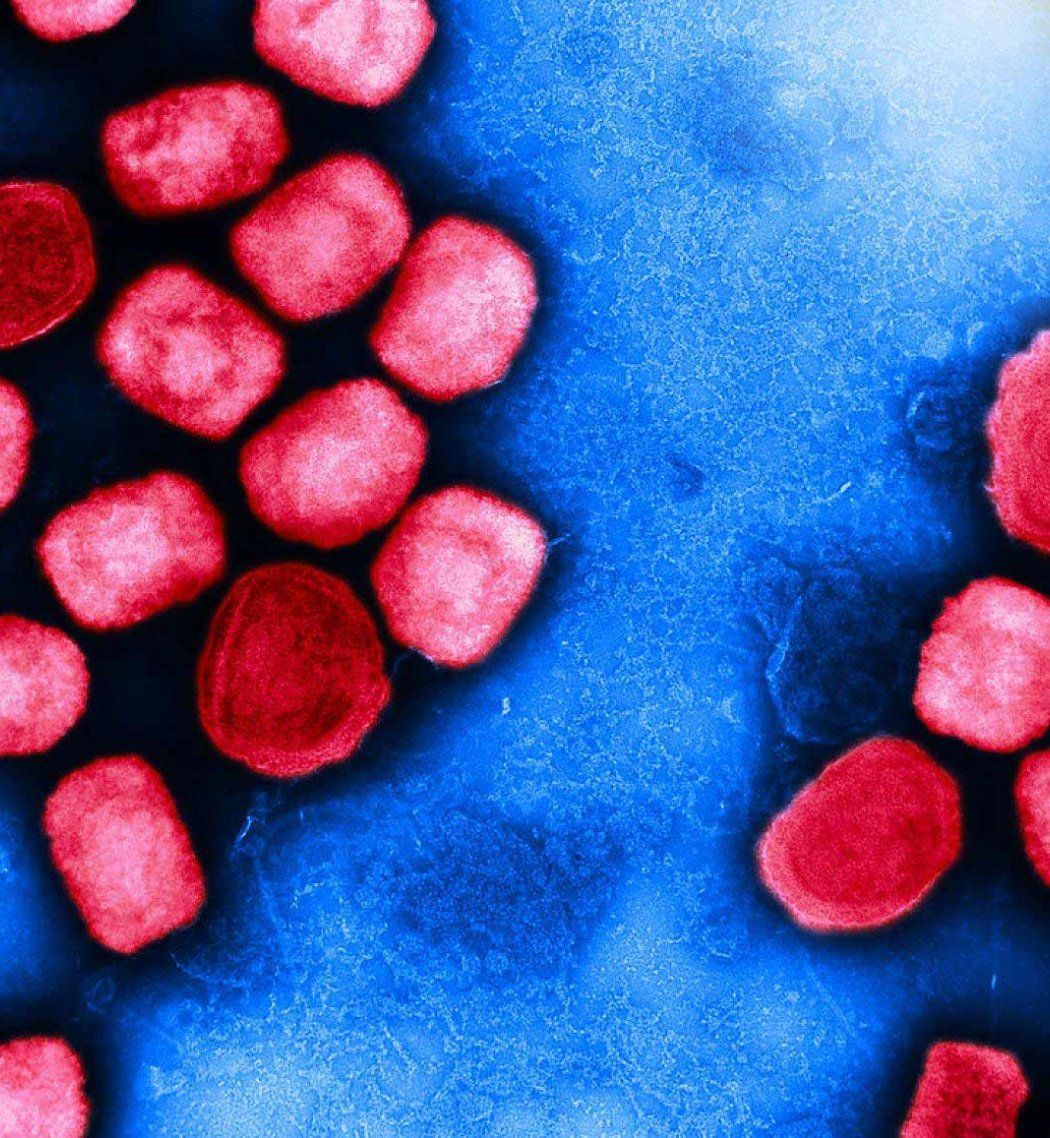
Mpox is a rare but dangerous viral infection in the same family of viruses as smallpox. Mpox symptoms are similar to chickenpox, with fevers, diarrhea, swollen lymph nodes and, most notably, skin lesions.
There are two strains of mpox, clade 1 and clade 2. Clade 1 is the more severe strain, with a fatality rate of 3.6%, that is currently spreading in Central and East Africa. Clade 2, with less severe illness and less than 0.2% fatality rate, was the strain responsible for the 2022 outbreak originating in West Africa.
Why did the WHO declare a global emergency?
The main reason for the declaration was the regional increase in the number of mpox cases and the spread to nearby countries in Central and East Africa. More information is needed to determine the cause of the increase and whether it represents a change in how the virus is transmitted. It is possible that some of the increased reported infections are due to heightened surveillance following the global 2022 mpox outbreak.
By declaring a global emergency, the WHO has put countries on notice of the public health risk in an effort to direct resources towards disease surveillance, mitigation efforts and clinical preparedness.
Is mpox the next pandemic?
Not at this time and unlikely in the near future because of the existing vaccines and anti-viral medications that can effectively stop the spread of the virus and reduce the severity in most cases.
How is mpox spread?
Mpox is spread by human-to-human contact if healthy skin comes in contact with infected skin lesions. The global mpox outbreak in 2022 demonstrated that mpox can spread through sexual encounters, particularly among men who have sex with men.
Mpox also spreads by animal-to-human contact, which could include being bitten by or cooking an infected animal. Historically a majority of clade I mpox was due to animal-to-human transmission.
Mpox is not a classic airborne disease but can be transmitted by recent contact with inanimate objects like infected clothing and bedsheets. The virus does not live long on inanimate objects and the most common transmission has been intimate contact.
When is mpox most contagious?
Mpox is most contagious when there are vesicles or boils on the skin.
Who is most at risk of getting mpox?
Vulnerable people living in high-density areas where mpox is known to exist, such as some refugee camps in Sub-Saharan Africa, are most susceptible to the disease. These individuals are also at higher risk of severe cases of the disease because they are often malnourished and have less access to health care. In the U.S., the risk of mpox infections is low because the prevalence of the disease is very low in this country. In addition, the U.S. has access to vaccines and antivirals to mitigate the disease.
That said, immunocompromised patients with HIV and those recovering from organ transplants, immunosuppressive chemotherapy or certain autoimmune diseases must be careful to avoid risky exposures. However, even for high-risk individuals, a greater concern than mpox is exposure from more prevalent infections like RSV, influenza and COVID-19.
Can mpox kill you?
Luckily, mpox has a lower mortality rate than the related smallpox virus. However, in the Democratic Republic of the Congo, the clade 1 case fatality rate has been estimated to be 3.6% this year. Those at greatest risk of dying are those without access to vaccinations and antivirals to manage the infection. If clade I came to the U.S., the case fatality rate in the would likely be much lower than that seen in Africa.
Is there a cure or vaccine for mpox?
Most cases of mpox resolve on their own. Treatment with antivirals like Tecovirimat (TPOXX) can reduce the severity of symptoms. The safest vaccine for the virus is Jynneos, which is effective at preventing infection with mpox – either from a recent exposure or from future exposures.