UC San Francisco scientists have found that SARS-CoV-2 can linger in the body for years and could be driving a global epidemic in long COVID.
They’re also exploring the surprising long-term risks of getting COVID in pregnancy.
Assistant Professor of Medicine Michael Peluso, MD, heads UCSF’s LIINC program, short for “Long-term Impact of Infection with Novel Coronavirus,” a university-wide effort to understand one of COVID-19’s most enduring challenges. Peluso and Professor of Pediatrics Valerie Flaherman, MD, MPH, lead components of the National Institutes of Health’s long COVID consortium, RECOVER – or Researching COVID to Enhance Recovery.
Peluso and Flaherman tell us what we know about long COVID – and what we don’t.
What is long COVID?
Peluso: There’s not a single picture of long COVID, and that’s one reason it’s been challenging to study.
Still, when clinicians or researchers talk about long COVID, they’re referring to medically unexplained symptoms that persist for months or years after somebody’s had COVID.
We don’t know what causes it, why this happens to some people and not others, or how to get people feeling better, which is what we spend most of our time trying to figure out.
What are some of the most common long COVID symptoms?
Peluso: Symptoms include “brain fog” – issues with memory or thinking – trouble breathing and fatigue. Fatigue doesn’t mean feeling a little tired – it’s bone-crushing fatigue, or what we refer to as post-exertional malaise.
Other common symptoms:
Other common symptoms:
- Mood changes
- Trouble concentrating
- Loss of taste or smell
- Coughing
- Joint pain
- Muscle aches
- Headaches
- Poor sleep
- Racing heart
- Chest pain
- Blood pressure issues
- Poor appetite
Post-exertional malaise occurs when a physical, cognitive or even social activity that a person used to be able to do easily causes debilitating fatigue for days afterward. It’s often best demonstrated by people who were quite fit before they got COVID – running miles or going on long hikes, for instance. Now, they can only do a fraction of that.
Some people also have prominent gastrointestinal symptoms like nausea, abdominal pain or diarrhea. We’re even seeing genitourinary symptoms like pelvic pain and menstruation issues.
Who is most at risk of long COVID?
Flaherman: Generally, people who have had a more severe COVID infection are at a higher risk for developing long COVID, as are elderly people, and those with pre-existing conditions or who have not been vaccinated.
What about pregnancy and long COVID?
Flaherman: We still don’t know for sure, but our data suggests that pregnant people may be at a lower risk of developing long COVID when we compare to the estimates we’re getting from the adult RECOVER cohort. Still, long COVID affects pregnant people in uniquely risky ways. Almost 1 in 10 pregnant people developed long COVID in our recent study done alongside the University of Utah. That study involved about 1,500 people who had contracted COVID during pregnancy.
The most common symptom was post-exertional malaise.
Can pregnant people pass the virus onto their fetuses?
Flaherman: It’s difficult to be certain, but if it is possible, it seems quite rare.
What about newborns?
Flaherman: If a pregnant person is infected with SARS-CoV-2 at the time of delivery, then it’s possible that she, like anyone else in the delivery room, could transmit the virus to the baby. We recommend that mothers who have SARS-CoV-2 around delivery wear a mask while holding or breastfeeding their baby and wash their hands frequently for five days after they have been fever-free.
Should new mothers with SARS-CoV-2 breastfeed?
Flaherman: Yes. Breastfeeding provides benefits to babies, including some immunity to SARS-CoV-2, which helps them fight off any COVID-19 that they might be exposed to. We encourage mothers to breastfeed babies directly, even if they have COVID-19, but to mask and wash their hands frequently.
When does long COVID go away?
Flaherman: In the pregnant people and new mothers we studied, those who developed long COVID had symptoms for nearly a year on average.
Peluso: Most of the data shows that this can go on for years and that the proportion of people who fully recover is disturbingly small. Sometimes, it’s as low as 10%.
What might be causing long COVID?
Peluso: If you had told me four years ago that we’d be having this conversation about SARS-Cov-2 persisting in people’s bodies, I wouldn’t have believed you.
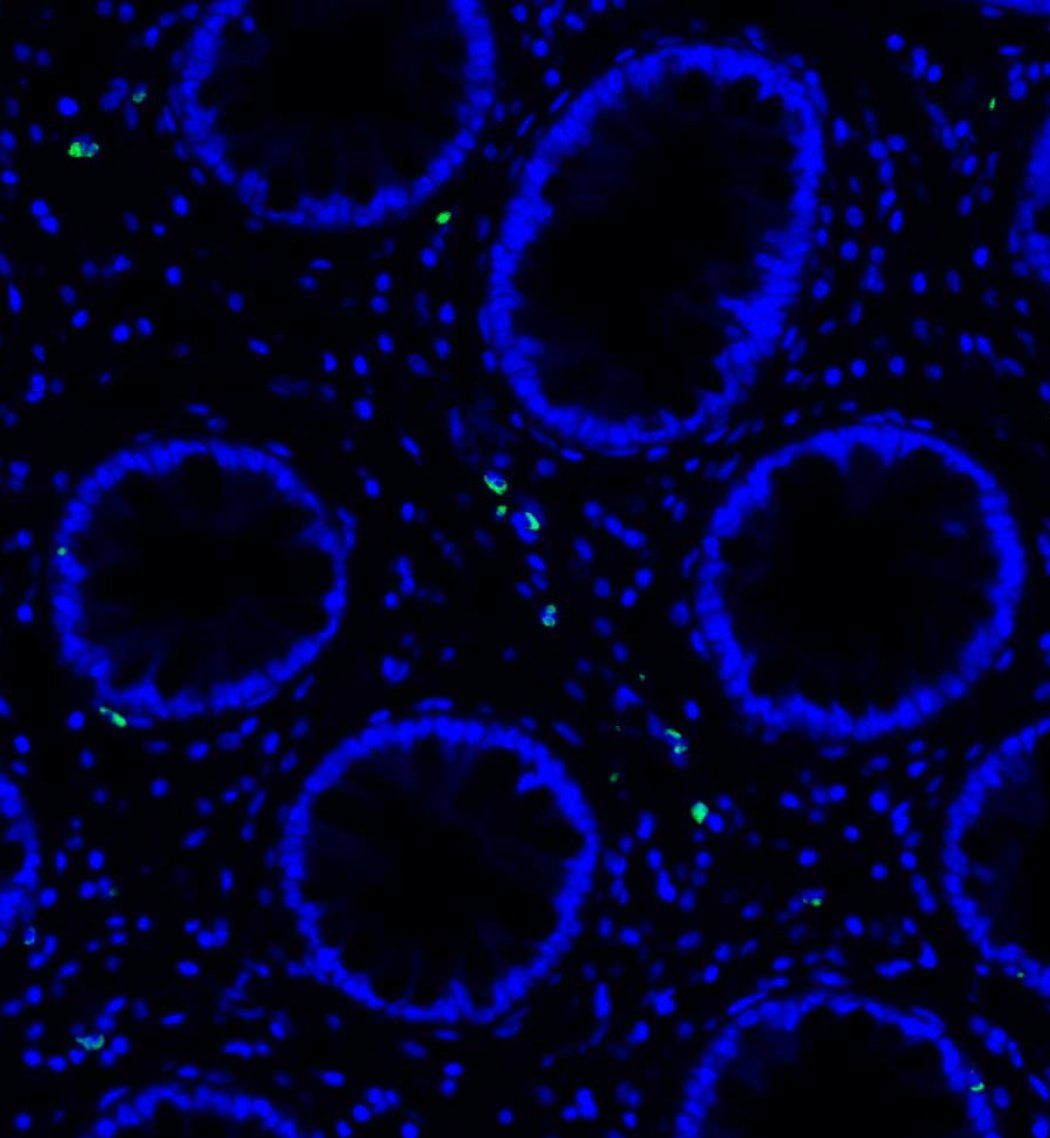
Recently, we reported that we could find SARS-CoV-2 protein in the blood of some people post-COVID. This must be coming from somewhere. Our hypothesis is that pieces of the virus persist in tissues and organs, so at UCSF, we started by looking at the GI tract of people with long COVID. This is relatively easy to do – as anyone who’s ever had a colonoscopy would know.
What we found was surprising. Some people with long COVID had pieces of the virus in their GI tract, even a year or two after they had COVID. And we at UCSF were the first to show that this virus could still be active.
Were the pieces of the virus you found replicating?
Peluso: We don’t know for sure yet. But we detected double-stranded RNA, which should only be present if the virus was moving through its lifecycle and replicating.
Why might SARS-CoV-2 be lingering in the body?
Peluso: One reason might be that the virus is in pockets cordoned off from the immune system. For example, immune cells might have walled it off as they worked to contain it. Another possibility is that it hides out in areas that are tougher to reach, like the nervous system. A third possibility is that the virus could evolve after infection so that the immune response is no longer effective against it.
You can imagine all sorts of scenarios. We don’t know which one is true yet. But this is a major lead that we are chasing down.
How can I reduce my risk of long COVID?
Peluso: Not getting COVID in the first place is the best strategy, but that’s easier said than done. I’m still quite diligent about masking and vaccination because studies have shown that being up to date with your vaccine when you get COVID-19 can reduce your risk of developing long COVID.
We don’t yet know if taking Paxlovid or an antiviral will reduce your risk of long COVID, but it could help you and is worth discussing with your doctor.
What are some of the most common long COVID symptoms?
Peluso: Symptoms include “brain fog” – issues with memory or thinking – trouble breathing and fatigue. Fatigue doesn’t mean feeling a little tired – it’s bone-crushing fatigue, or what we refer to as post-exertional malaise.
Post-exertional malaise occurs when a physical, cognitive or even social activity that a person used to be able to do easily causes debilitating fatigue for days afterward. It’s often best demonstrated by people who were quite fit before they got COVID – running miles or going on long hikes, for instance. Now, they can only do a fraction of that.
Some people also have prominent gastrointestinal symptoms like nausea, abdominal pain or diarrhea. We’re even seeing genitourinary symptoms like pelvic pain and menstruation issues.
Other common symptoms:
Other common symptoms:
- Mood changes
- Trouble concentrating
- Loss of taste or smell
- Coughing
- Joint pain
- Muscle aches
- Headaches
- Poor sleep
- Racing heart
- Chest pain
- Blood pressure issues
- Poor appetite
Who is most at risk of long COVID?
Flaherman: Generally, people who have had a more severe COVID infection are at a higher risk for developing long COVID, as are elderly people, and those with pre-existing conditions or who have not been vaccinated.
What about pregnancy and long COVID?
Flaherman: We still don’t know for sure, but our data suggests that pregnant people may be at a lower risk of developing long COVID when we compare to the estimates we’re getting from the adult RECOVER cohort. Still, long COVID affects pregnant people in uniquely risky ways. Almost 1 in 10 pregnant people developed long COVID in our recent study done alongside the University of Utah. That study involved about 1,500 people who had contracted COVID during pregnancy.
The most common symptom was post-exertional malaise.
Can pregnant people pass the virus onto their fetuses?
Flaherman: It’s difficult to be certain, but if it is possible, it seems quite rare.
What about newborns?
Flaherman: If a pregnant person is infected with SARS-CoV-2 at the time of delivery, then it’s possible that she, like anyone else in the delivery room, could transmit the virus to the baby. We recommend that mothers who have SARS-CoV-2 around delivery wear a mask while holding or breastfeeding their baby and wash their hands frequently for five days after they have been fever-free.
Should new mothers with SARS-CoV-2 breastfeed?
Flaherman: Yes. Breastfeeding provides benefits to babies, including some immunity to SARS-CoV-2, which helps them fight off any COVID-19 that they might be exposed to. We encourage mothers to breastfeed babies directly, even if they have COVID-19, but to mask and wash their hands frequently.
When does long COVID go away?
Flaherman: In the pregnant people and new mothers we studied, those who developed long COVID had symptoms for nearly a year on average.
Peluso: Most of the data shows that this can go on for years and that the proportion of people who fully recover is disturbingly small. Sometimes, it’s as low as 10%.
What might be causing long COVID?
Peluso: If you had told me four years ago that we’d be having this conversation about SARS-Cov-2 persisting in people’s bodies, I wouldn’t have believed you.
Recently, we reported that we could find SARS-CoV-2 protein in the blood of some people post-COVID. This must be coming from somewhere. Our hypothesis is that pieces of the virus persist in tissues and organs, so at UCSF, we started by looking at the GI tract of people with long COVID. This is relatively easy to do – as anyone who’s ever had a colonoscopy would know.
What we found was surprising. Some people with long COVID had pieces of the virus in their GI tract, even a year or two after they had COVID. And we at UCSF were the first to show that this virus could still be active.
Were the pieces of the virus you found replicating?
Peluso: We don’t know for sure yet. But we detected double-stranded RNA, which should only be present if the virus was moving through its lifecycle and replicating.
Why might SARS-CoV-2 be lingering in the body?
Peluso: One reason might be that the virus is in pockets cordoned off from the immune system. For example, immune cells might have walled it off as they worked to contain it. Another possibility is that it hides out in areas that are tougher to reach, like the nervous system. A third possibility is that the virus could evolve after infection so that the immune response is no longer effective against it.
You can imagine all sorts of scenarios. We don’t know which one is true yet. But this is a major lead that we are chasing down.
How can I reduce my risk of long COVID?
Peluso: Not getting COVID in the first place is the best strategy, but that’s easier said than done. I’m still quite diligent about masking and vaccination because studies have shown that being up to date with your vaccine when you get COVID-19 can reduce your risk of developing long COVID.
We don’t yet know if taking Paxlovid or an antiviral will reduce your risk of long COVID, but it could help you and is worth discussing with your doctor.