UCSF Scientists Win Pew Awards for Cancer and Neuroscience Research
Funds will allow them to pursue questions related to learning and reward, cell therapies for cancer, and cancer genetics.
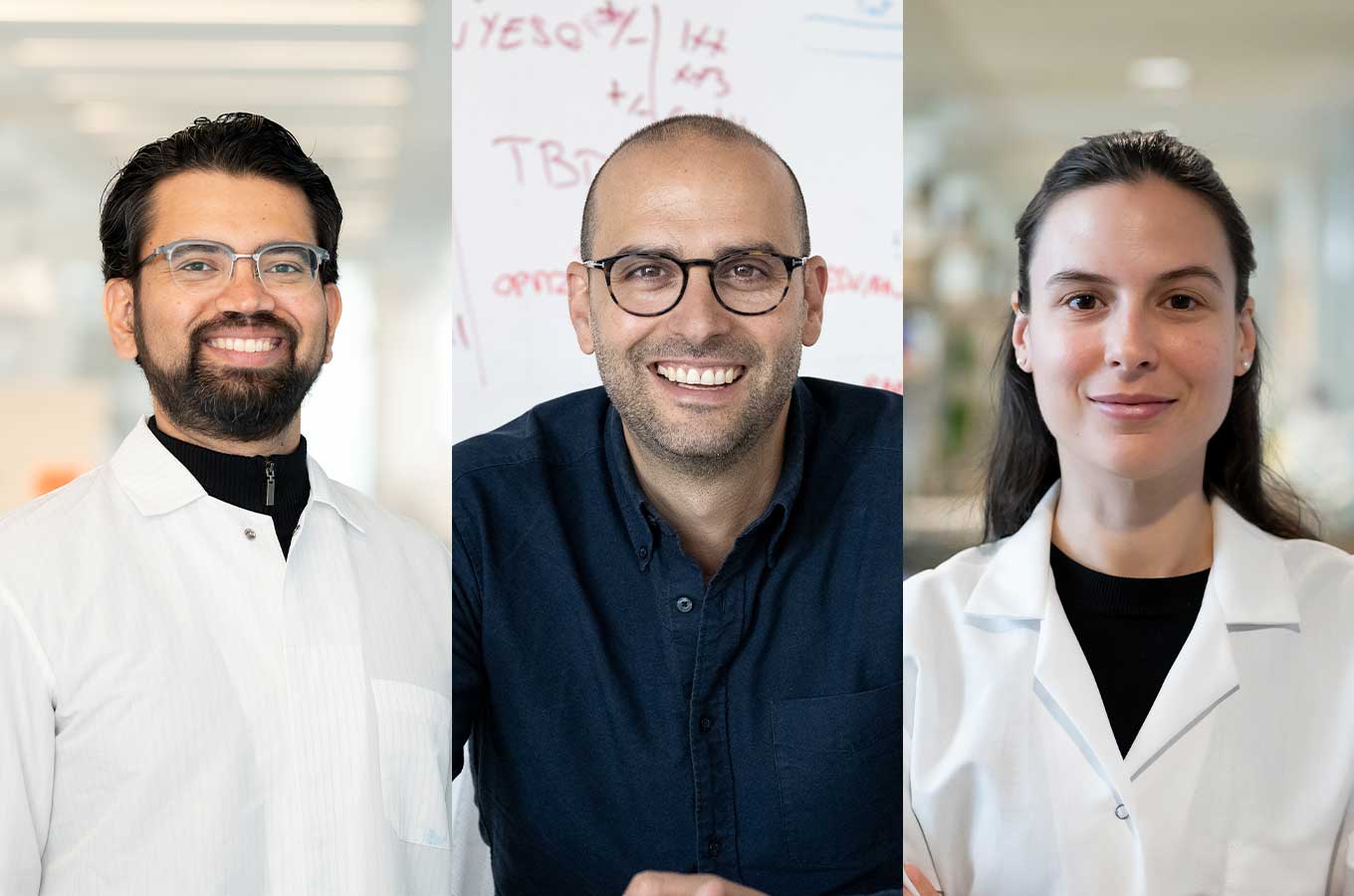
Three UC San Francisco scientists have received 2024 Pew awards to fund their research in neuroscience and cancer.
They include a cognitive scientist, Vijay Mohan K Namboodiri, PhD, who is challenging the reigning theory of learning; Justin Eyquem, PhD, a bioengineer who aims to build cancer-fighting cell therapies from within a person’s body; and Jovanka Gencel-Augusto, PhD, a postdoctoral scholar from Peru who is studying cancer genetics.
What really happens in learning?
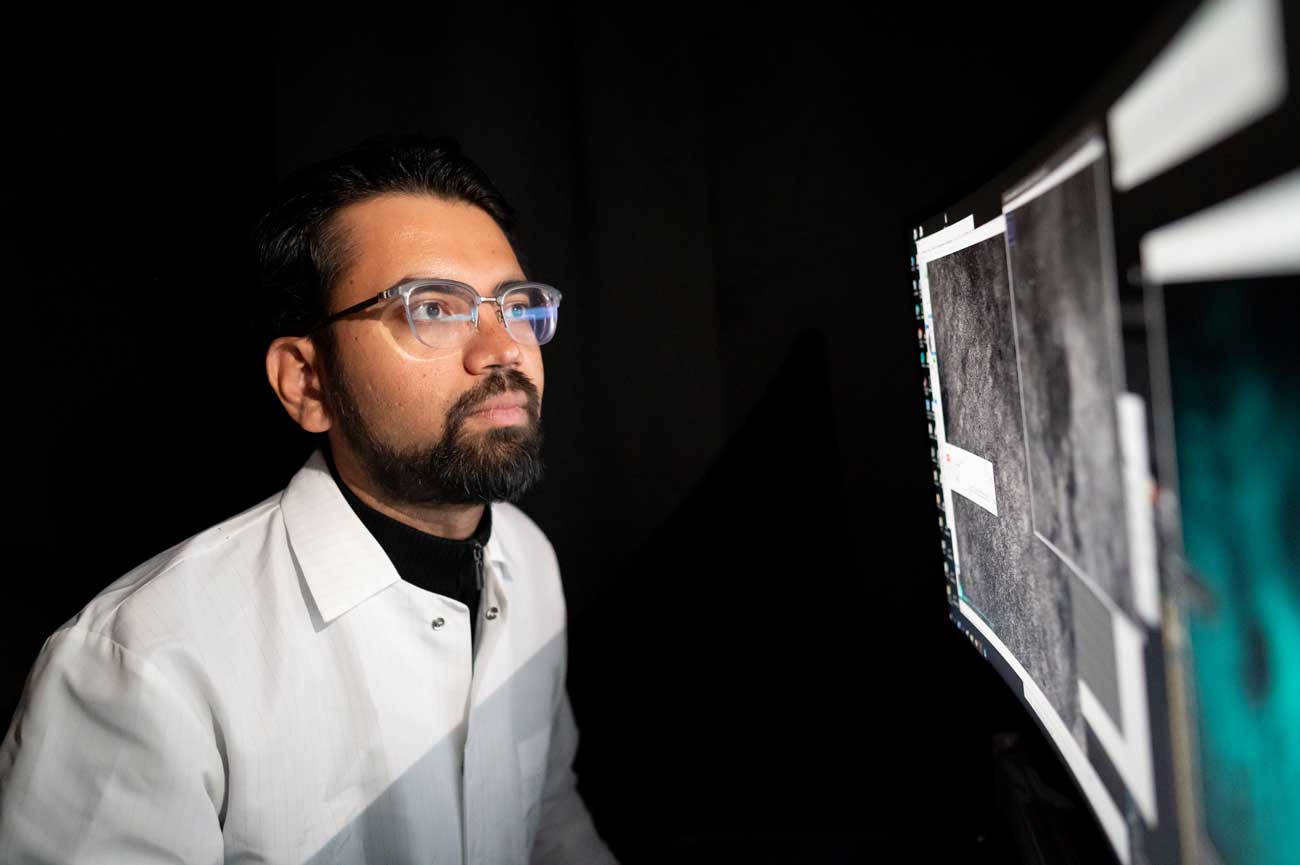
Namboodiri, a Pew Scholar in the Biomedical Sciences, studies the role that dopamine plays in associative learning, the process that connects cause with effect.
In other words, if you eat at a restaurant and don’t feel well afterward, how does your brain translate that into, “Don’t eat there again”?
The current consensus is that animals continuously predict what will happen in a given situation, and when they are wrong, a dose of dopamine in their brains marks the error and helps the animal refine its understanding.
But the process may actually work in reverse. Namboodiri has uncovered evidence that noteworthy experiences, rather than erroneous predictions, trigger the dopamine hits, causing the animal to think back on what might have caused them.
Namboodiri will use the four-year fellowship to map the location and activity of each individual neuron involved in this process in mice. Understanding exactly what is happening in these learning-and-reward systems could point the way to resetting them when they become impaired in disorders such as addiction and PTSD.
“Being able to predict an outcome is one of the most fundamental aspects of animal life,” said Namboodiri. “My hope is that this work brings us a new understanding about how animal brains learn.”
A new way to engineer cells in the body
Eyquem, a Pew-Stewart Scholar for Cancer Research, is a bioengineer who has been refining a sophisticated cancer treatment called CAR-T therapy, in which a patient’s own immune cells are re-engineered to attack the tumor.
While these treatments can be highly successful, living drugs are also difficult to make and prohibitively expensive.
The process involves isolating immune cells from patients’ blood and reprogramming them with gene editing, which must be done in a sterile facility. The cells are only put back in after patients have undergone chemotherapy to suppress their immune systems.
Eyquem wants to skip over these steps with technologies that can edit immune cells directly within a person’s body.
This innovation could eliminate costly steps in the production of the cells and spare patients from needing chemotherapy. Eyquem hopes this will make CAR-T cell therapy dramatically cheaper, faster and more accessible.
Eyquem is part of a small cohort of Pew-Stewart scholars who will meet throughout the four-year fellowship to share their work and hopefully inspire new ideas.
“It’s going to introduce me to a community of very creative thinkers and people that are at the forefront of this field,” he said. “This is the kind of network that really helps move these discoveries from the lab into the clinic.”
A tumor suppressing gene that malfunctions
Gencel-Augusto, a Pew Latin American Fellow in the Biomedical Sciences, works in the labs of Jennifer Grandis, MD, and Daniel Johnson, PhD, where she is bringing her expertise in genetics and cancer biology to study p53, a gene that helps prevent tumors and is often altered in head and neck cancers. She hopes to pinpoint exactly how p53 keeps tumors at bay and find ways to reactivate it when it gets compromised.
Growing up in the small town of Piura, Peru, Gencel-Augusto developed a passion for her field when her maternal aunt was diagnosed with breast cancer at the age of 36. Gencel-Augusto moved to the capital city of Lima to get a degree in biology, and learned about genetic testing for breast cancer while doing an internship with a local cancer institute that was partnered with the Mayo Clinic.
Her aunt tested positive for BRCA1, a gene that increases risk for breast and ovarian cancer and is often treated in the United States with a preventative mastectomy. Her aunt’s doctors never recommended it, however, and her cancer came back five years later. For Gancel-Augusto, the experience highlighted how the lack of resources and knowledge in Peru affects people’s health.
Gencel-Augusto moved to the U.S. for her PhD, and she is grateful to have landed a postdoctoral position at UCSF. Her dream, she said, is to have her own lab where she trains Latin American scientists in cancer research.
“That’s the whole motivation for my career,” she said. “I want to contribute to improving cancer research and the situation for cancer patients back home.”
