How 3D Printer Heart Technology Changed a Teen’s Life
Surgeons can now pinpoint heart disease thanks to recent advances in modeling
At 3 weeks old, Samantha underwent the first of four surgeries for congenital single-ventricle heart disease. She had been diagnosed before birth with the rare birth defect that left only half of her heart to pump, and a plan was made then for her to undergo two more surgeries over the course of her childhood to reconfigure her circulation to function as normally as possible.
Samantha’s second and third surgeries, at 1 and 6 years old, improved her blood flow by replumbing her single-ventricle heart to increase the flow of oxygen in her bloodstream. Functioning on a single ventricle was a short-term solution, though, and over the long term could cause liver disease, heart failure and, potentially, require a pacemaker and heart transplant in adulthood.

“ ... Her care at UCSF has changed her life and allowed her to live like a normal kid. She can do just about anything and we are so proud of her.”
Samuel Rodriquez, Samantha’s father
A quandary arose after the third surgery because Samantha was stable and living a fairly normal life. Should they proceed with a fourth surgery? The high-risk procedure to restructure her heart had the possibility of being a lifetime cure, but was also extremely delicate and a risk for a child who was not severely compromised by the shortage of oxygen in her bloodstream.
“We wanted to give her every opportunity to live her best life,” said Samantha’s father, Samuel Rodriquez. “She has always been a fighter and she deserved a chance.”
At 12 years old, Samantha’s parents and her cardiac team at UCSF Benioff Children’s Hospitals’ Pediatric Heart Center made the decision to re-evaluate her condition using high-precision technology at the UCSF Center for Advanced 3D+ Technologies (CA3D+). Using data from high-resolution 3D imaging, the CA3D+ team produced a 3D printed model – an exact replica of Samantha’s heart – that accurately pinpointed her heart abnormalities and enabled them to evaluate whether she could undergo a two-ventricle repair.
“3D-heart models provide a level of understanding of a patient’s anatomy that has never before been possible,” said Shafkat Anwar, MD, pediatric cardiologist and medical director of the UCSF Center for Advanced 3D+ Technologies. “During surgery every minute matters. These models provide a much richer and more detailed conversation about how to fix problems before entering the operating room.”

“3D-heart models provide a level of understanding of a patient’s anatomy that has never before been possible.”
How to Practice Heart Surgery
With life-sized heart models printed on materials as soft as skin or as tough as bone, surgeons can assess the best surgical route and even practice the surgery to determine the best course of action prior to an operation. Samantha’s surgical team, led by Mohan Reddy, MD, used the heart to assess a safe path to successfully reconfigure her single ventricle heart into two fully functioning ventricles.
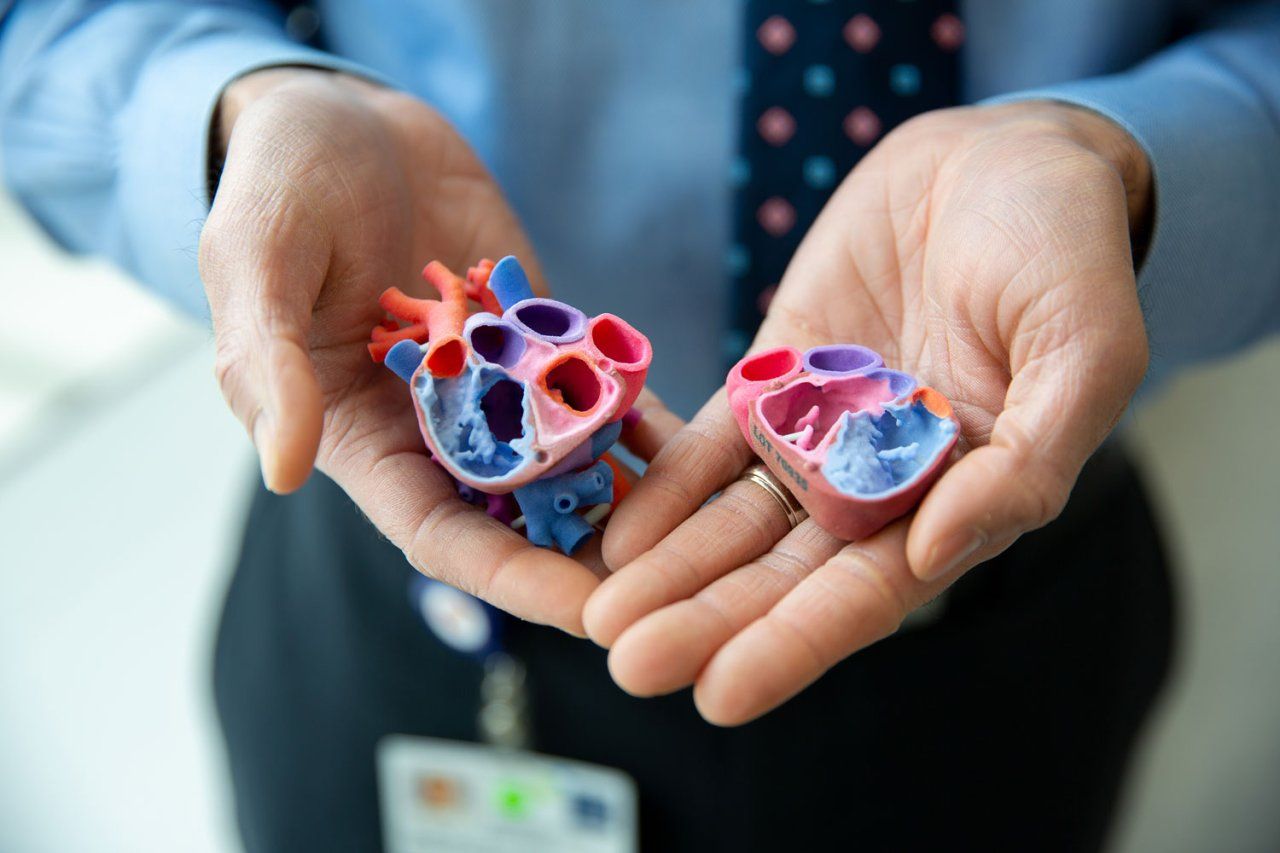
Re-evaluating Samantha’s prognosis with the newest technology was in keeping with her medical team’s commitment to provide the best possible outcomes for her and other patients with similar heart conditions. Anwar, Reddy and Samantha’s cardiologist, Mark Cocalis, MD, collaborated to design her surgery using the 3D heart model, which enabled them to determine with accuracy if the surgery had a good chance of success.
“Very few cardiac programs would have taken on this type of high-risk surgery,” Anwar said. “Since she was otherwise stable, many would have left well enough alone. But we knew giving Samantha a heart with two functioning pumping chambers and a more normal circulation would ultimately give her a better outcome.”
Samantha’s physical endurance has improved dramatically following her fourth surgery. While previously winded and sitting on the sidelines during soccer practice, the 15-year-old now is able to keep up with her friends in swimming and biking, when she is not volunteering to work with infants and toddlers at her local Head Start center.
“Enduring so many surgeries was hard for Samantha and hard for the family, but her care at UCSF has changed her life and allowed her to live like a normal kid,” Samuel said. “She can do just about anything and we are so proud of her.”