Why Experts Are Urging Social Distancing to Combat Coronavirus Outbreak

Editor’s Note: This story was updated on Mar. 16 to reflect the President's Coronavirus Guidelines for America and orders by Bay Area counties to shelter in place.
As cities and towns across the United States confront the growing number of COVID-19 cases, epidemiologists say we are now in the mitigation phase of the outbreak. The virus is already in our communities, so the focus now is to mitigate, or reduce, the damage from the disease.
The news is full of reports about cities canceling events and closing schools as well as businesses urging employees to work from home if possible.
UC San Francisco epidemiologists Jeff Martin, MD, MPH, and George Rutherford, III, MD, explained why these public health measures are being taken and what each of us can do to slow the outbreak and help to save lives.
Above all, keep your distance.
“‘Social distancing’ will be the key phrase in the days and weeks to come,” said Martin. The term simply refers to avoiding close contact with other individuals in order to avoid catching the virus yourself and to avoid passing it on.
Social distancing is currently the most important factor we can control in the COVID-19 outbreak, and therefore critical, explained Martin. Many factors contribute to the so-called reproductive number of the new coronavirus, which describes roughly how many people an infected individual will go on to infect. Currently, estimates of the reproductive number of the novel coronavirus range from 1.4 to 6.5, with an average of 3.3.
“The higher the reproductive number, the faster it will spread,” said Martin. Factors that affect the reproductive number include how inherently contagious the virus is, how susceptible people are to infection, the number of contacts between people, and the duration of those contacts.
Social distancing now is one of the greatest calls for altruism.
“We’re not at a stage to modify the first two factors – the biologic behavior of the virus or the susceptibility of individuals – but each of us can decrease the number and duration of our contacts with others,” said Martin.
Social distancing can also effectively extend to environmental precautions such as disinfecting often-touched surfaces that may pass on the virus, said Martin. He offered a phrase borrowed from camping, “leave no trace behind,” when practicing these precautions.
What social distancing means in daily life.
Many cities have encouraged social distancing by banning large gatherings, encouraging telecommuting and closing schools. Rutherford advised avoiding crowded public transportation if possible. Social activities are now discouraged, but what does social distancing mean for essential activities? Those decisions may depend on your age and susceptibility to infection. “If you’re over 60, you should be laying low, staying home,” said Rutherford.
For younger people, Martin pointed out that anyone who becomes infected can spread the virus to an older person or someone who is immunocompromised. "So, the fewer young persons who become infected, the lower the incidence in the older population," he said.
According to the President's Coronavirus Guidelines for America, everyone should avoid social gatherings of more than 10 people, and avoid eating or drinking at bars, restaurants, and food courts. If someone in your household has tested positive for the coronavirus, keep the entire household at home.
In the Bay Area, a number of counties including San Francisco have issued orders to shelter in place from March 17, 2020, through April 7, 2020. Everyone should stay at home except for certain essential activities, such as grocery shopping or to seek medical care, or to perform work for essential businesses, government agencies, or public infrastructure construction.
What experts fear most: an overwhelmed health care system.
Epidemiologists said the fear now is that a sudden surge in patients needing critical medical care will over-burden the health care system. “If the outbreak is unchecked, if we did nothing, you would see a rapid escalation of infections, and that peak is what overwhelms health care systems,” said Martin.
“Flattening the curve” means dampening down that peak by reducing how fast the virus moves through the population. A slower spread means that on any given day, fewer people will need critical care for severe illness. The best way to slow the spread is through public health measures that encourage social distancing.
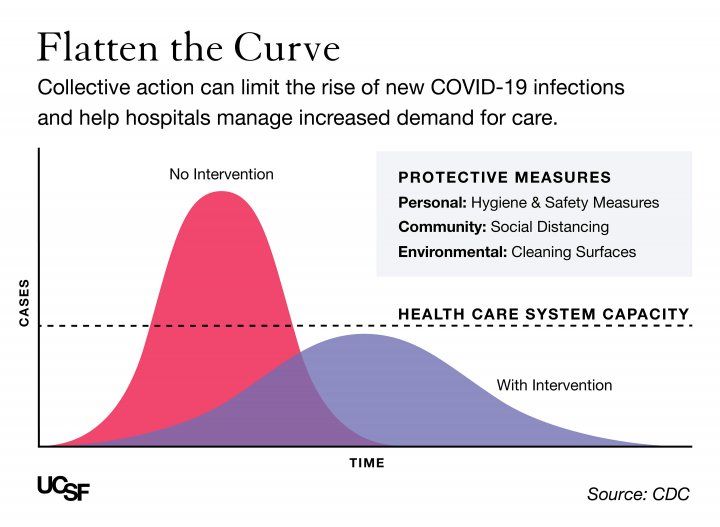
According to some experts, more than 120 million Americans eventually may be infected with COVID-19, though Rutherford believes these estimates to be high. If 2 million were in critical condition, that could easily surpass the 98,000 intensive care unit beds and 62,000 full-feature ventilators available in the U.S. “If they all came in the same week, the results could be catastrophic,” said Rutherford. “But if that can be spread out over 40 weeks, it’s more like 50,000 critical cases a week and more within our range to handle.”
Martin added that getting a flu shot, which lowers your chances of getting and spreading the flu, is another way to help lighten the burden on the health care system during this critical time.
When should you call a doctor?
The two symptoms most commonly associated with COVID-19 are fever and a dry cough. “One without the other is less common, though not impossible. Having both is more typical for COVID-19 infection,” said Martin. In contrast, a common cold often starts with sore throat, runny nose and sneezing, without much fever or cough. The seasonal flu comes with fever and cough but is more likely also to feature muscle ache, according to Martin.
Many people think they have a fever without taking their temperature, said Rutherford. “Get a thermometer,” he said. “Take your temperature.”
If you have shortness of breath, a more serious symptom of COVID-19 that may be a sign of pneumonia, you should not wait to seek medical attention, said Martin.
If you have symptoms suggestive of COVID-19, especially if you have traveled to an affected area or contact with someone who has, call your doctor or clinic first so they can be prepared if you need to come in.
This is not “just a bad flu.”
COVID-19 is more serious than the seasonal flu in several ways. Unlike the flu, there is no known treatment or vaccine for COVID-19. The overall case fatality rate may be 1 to 2 percent, which is 10 to 20 times higher than that of the flu.
We may also be more susceptible to the novel coronavirus because humans have never encountered it before, unlike strains of the flu that often circulate. When it comes to specific immunity against the new virus, “we’re all running naked,” said Martin. He speculated that more generic forms of "innate" immunity may be responsible for younger individuals having an easier time avoiding disease.
The young and healthy have a critical role to play.
“Social distancing now is one of the greatest calls for altruism,” said Martin. “People aren’t asked to do this to protect themselves, it’s really to protect those who are most susceptible.” Data from tens of thousands of cases in China suggests that the severity of COVID-19 increases dramatically with older age and for those with underlying health conditions. The death rate for infected patients in their 80s was about 15 percent in the Chinese study.
“People need to understand that this is really, really serious,” said Rutherford. “It’s up to you to not get infected and to not infect others. Prevent infection by staying in your house, washing your hands, avoiding people who are sick. Society needs your help.”
“I realize the advice is difficult to do,” he added, “But it’s life-saving – not necessarily for you if you are 30 years old and healthy, but maybe for your parents, and certainly for your grandparents.”

UCSF Coronavirus Resources
Information for the UCSF community, including procedures, guidance for travelers, and latest updates.