Immune Cells in Spinal Fluid of Multiple Sclerosis Patients Identified as Likely Disease Drivers
Results Lay Groundwork for New, More Targeted Immune Therapies
New UC San Francisco research sheds light on how immune system B cells that infiltrate the central nervous system may drive multiple sclerosis (MS), pointing the way to a new generation of targeted immune therapies to halt the progression of the disease.
MS is a common autoimmune neurological disease affecting approximately 1 million Americans. It is caused when the immune system mistakenly attacks nerve cells’ crucial insulating layer, called myelin, resulting in loss of muscle control and ultimately degeneration of the nervous system.
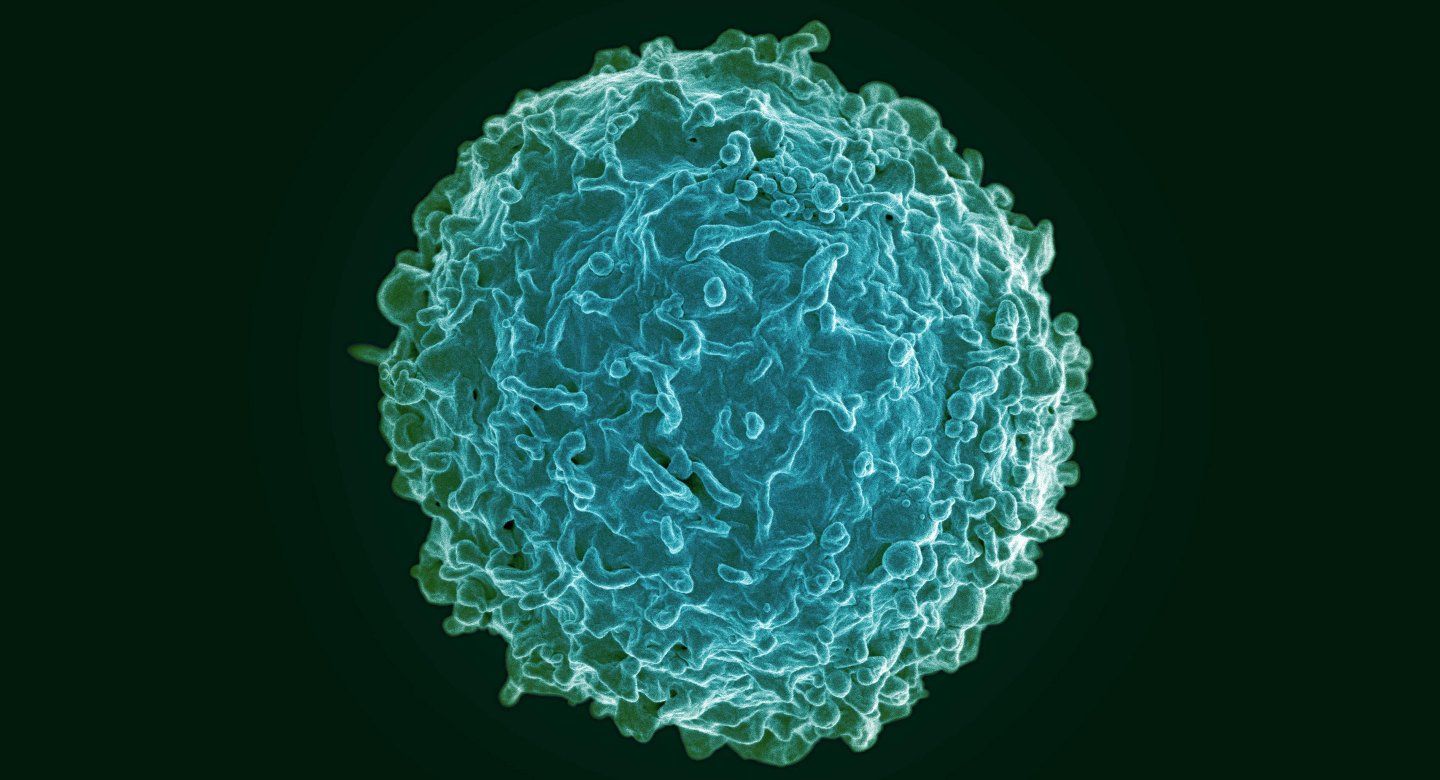
The cause of MS is unknown, but recent evidence points to an important role for B cells, which act as the immune system’s “memory,” responsible for producing antibodies and recruiting other immune cells to fend off previously encountered pathogens. Scientists hypothesize that, in MS patients, some as yet unknown event triggers B cells to begin coordinating an immune assault on myelin.
Recent therapeutic breakthroughs led by Stephen Hauser, MD, director of the UCSF Weill Institute for Neurosciences, have shown that depleting B cells can quickly eliminate debilitating episodes of numbness and paralysis in MS called relapses. However, these treatments do not completely eliminate B cells, particularly from the brain and spinal cord, and many patients continue to experience a gradual progression of their disease over years and decades.
“A longstanding question in the field of MS has been simply this: what are B cells doing in the spinal fluid of MS patients and why are they so difficult to remove even with our best available B cell removal treatments?” said Ryan Schubert, MD, one of the study’s lead authors, who conducted the work as a postdoctoral researcher in UCSF’s Department of Neurology. Schubert is now at Asceneuron, a Swiss biotech firm.
“The success of these therapies is nearly unprecedented in medicine, but the exact role of these B cells in MS is still poorly understood,” added postdoctoral researcher Akshaya Ramesh, PhD, the study’s other lead author. “We wanted to understand if certain populations of B cells play a particularly important role in the disease and might be targeted by future therapies.”
Their new paper – published Aug. 28 in Proceedings of the National Academy of Sciences (PNAS) – has for the first time comprehensively profiled gene activity in B cells within the central nervous systems of MS patients in an effort to understand exactly how these cells promote neurodegeneration. The study compared B cells from blood and spinal fluid of 23 patients with early-stage, untreated MS enrolled in the UCSF EPIC and ORIGINS studies, in an effort to understand how B cells initially infiltrate the central nervous system and trigger neurodegeneration.
“By identifying particular B-cell biological pathways that are more pronounced in in the spinal fluid of patients with MS, we hope to provide guideposts for development of next-generation B cell therapies,” said study senior author Michael Wilson, MD, an associate professor of neurology in the in the Division of Neuroimmunology and Glial Biology at the UCSF Weill Institute for Neurosciences.
Specifically, the researchers found that the spinal fluid of MS patients contains an abnormal number of mature, previously activated B cells, and that these cells showed significantly increased activation of certain genetic pathways linked to inflammation and to cholesterol metabolism, a biological pathway that had previously been hypothesized to have a role in MS.
“We see that B cells in the spinal fluid specifically turn on genes that increase their chance of surviving as they encounter brain and spinal fluid tissue, perpetuating a cycle of injury and resulting in the characteristic feature of MS – demyelination,” said Schubert.
Most enticingly, the researchers were able to sequence the surface protein on mature B cells that indicates what had previously activated them. Knowing the sequence of this protein, called the B Cell Receptor (BCR), on cells linked to autoimmunity in MS patients could potentially allow researchers to design highly targeted antibody drugs to eliminate just these “bad actor” B cells from patients. The information could also allow researchers to finally identify the specific molecules that may have triggered MS patients’ immune systems to attack their nerve insulation in the first place.
“If we could do that, we could design therapies to selectively deplete B cells that are reacting to this particular antigen or group of antigens,” Wilson said. “It would be the first opportunity to really go after the root cause of the disease.”