New CRISPR-Based COVID-19 Test Kit Can Diagnose Infection in Less Than an Hour
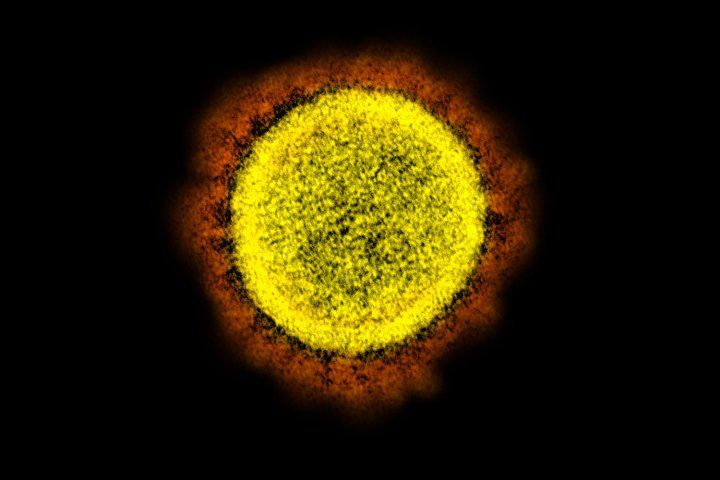
Transmission electron micrograph of the SARS-CoV-2 virus. Image credit: NIAID
Scientists have developed an inexpensive new test that can rapidly diagnose COVID-19 infections, a timely advance that comes as clinicians and public health officials are scrambling to cope with testing backlogs while the number of cases continues to climb.
Developed at UC San Francisco and Mammoth Biosciences, the new test – officially named the “SARS-CoV-2 DETECTR” – is easy to implement and to interpret, and requires no specialized equipment, which is likely to make the test more widely available than the current crop of COVID-19 test kits. Though the new test has yet to receive formal approval for clinical use from the U.S. Food and Drug Administration, UCSF researchers are clinically validating the test in an effort to fast-track the approval process through a so-called Emergency Use Authorization.
“The introduction and availability of CRISPR technology will accelerate deployment of the next generation of tests to diagnose COVID-19 infection,” said Charles Chiu, MD, PhD, professor of laboratory medicine at UCSF and co-lead developer of the new test, which is described in a paper published April 16, 2020, in the journal Nature Biotechnology.
The new SARS-CoV-2 DETECTR assay is among the first to use CRISPR gene-targeting technology to test for the presence of the novel coronavirus. Since CRISPR can be modified to target any genetic sequence, the test kit’s developers “programmed” it to home in on two target regions in the genome of the novel coronavirus. One of these sequences is common to all “SARS-like” coronaviruses, while the other is unique to SARS-CoV-2, which causes COVID-19. Testing for the presence of both sequences ensures that the new DETECTR tool can distinguish between SARS-CoV-2 and closely related viruses.

Charles Chiu, MD, PhD
Much like the diagnostic kits currently in use, the new test can detect the novel coronavirus in samples obtained from respiratory swabs. However, the new test is able to provide a diagnosis much more quickly. While the widely used tests based on polymerase chain reaction (PCR) techniques take about four hours to produce a result from a respiratory sample, the new DETECTR test takes only 45 minutes, rapidly accelerating the pace of diagnosis.
Another key advantage of the new DETECTR test is that it can be performed in virtually any lab, using off-the-shelf reagents and common equipment. This stands in stark contrast to PCR-based tests, which require expensive, specialized equipment, limiting those tests to well-equipped diagnostic labs. Plus, the new DETECTR test is easy to interpret: much like a store-bought pregnancy test, dark lines that appear on test strips indicate the presence of viral genes.
The new test is also highly sensitive. It can detect the presence of as few as 10 coronaviruses in a microliter of fluid taken from a patient – a volume many hundreds of times smaller than an average drop of water. Though slightly less sensitive than existing PCR-based tests, which can detect as few as 3.2 copies of the virus per microliter, the difference is unlikely to have a noticeable impact in diagnosis, as infected patients typically have much higher viral loads.
The SARS-CoV-2 DETECTR adds to a rapidly growing suite of new COVID-19 diagnostic tests that researchers and clinicians hope will increase testing capacity, including tests for specific antibodies in patients who have recovered from COVID-19 infection.
As researchers work to validate the new DETECTR test for FDA approval, its developers are continuing to make modifications to the test kit so that it can be used for field testing at sites like airports, schools, and small clinics.
Authors: James P Broughton of Mammoth Biosciences and Xianding Deng of UCSF are co-lead authors of the study. Charles Chiu of UCSF and Janice Chen of Mammoth Biosciences are co-senior authors of the study. Additional authors include Guixia Yu, Venice Servellita, Jessica Streithorst, Andrea Granados, Alicia Sotomayor-Gonzalez, Allan Gopez, Elaine Hsu, Wei Gu, and Steve Miller, and Kelsey Zorn, of UCSF; Clare L Fasching, Jasmeet Singh, and Xin Miao of Mammoth Biosciences; and Chao-Yang Pan, Hugo Guevara, and Debra Wadford of the California Department of Public Health.
Funding: This work was supported by National Institutes of Health (NIH) grants R33-AI129455 from the National Institute of Allergy and Infectious Diseases and R01-HL105704 from the National Heart, Lung, and Blood Institute; the Charles and Helen Schwab Foundation; and Mammoth Biosciences, Inc.
Disclosures: Chiu is the director of the UCSF-Abbott Viral Diagnostics and Discovery Center (VDDC), receives research support funding from Abbott Laboratories, and is on the Scientific Advisory Board of Mammoth Biosciences, Inc. Chen is a co-founder of Mammoth Biosciences, Inc. Broughton, Fasching, Singh, and Miao are employees of Mammoth Biosciences, Inc. Chiu, Broughton, Deng, Fasching, Singh, Miao and Chen are co-inventors of CRISPR-related technologies.
About UCSF: The University of California, San Francisco (UCSF) is exclusively focused on the health sciences and is dedicated to promoting health worldwide through advanced biomedical research, graduate-level education in the life sciences and health professions, and excellence in patient care. UCSF Health, which serves as UCSF's primary academic medical center, includes top-ranked specialty hospitals and other clinical programs, and has affiliations throughout the Bay Area.