Superfast Gene Sequencing Helps Diagnose Critically Ill Patients
‘Metagenomic’ Test for Neurological Infections Has Real Clinical Benefit, Says New Study
In an analysis of the real-world impact of a pioneering test called metagenomic next-generation sequencing (mNGS), developed by UC San Francisco scientists to diagnose patients with mysterious inflammatory neurological conditions, the technique was shown to identify infections better than any standard clinical method.
“The infectious cause of half the cases of meningitis and encephalitis go undiagnosed in hospitals around the country, and these severely ill patients are in dire need of a better testing tool”, said Charles Chiu, MD, PhD, professor of laboratory medicine and medicine at UCSF and senior author of the new study. Unlike conventional testing, which is often driven by doctors’ hunches, the mNGS test offers an unbiased approach that can detect nearly all possible pathogens – bacteria, viruses, fungi and parasites – present in patients’ spinal fluid, giving doctors clear direction for treatment.
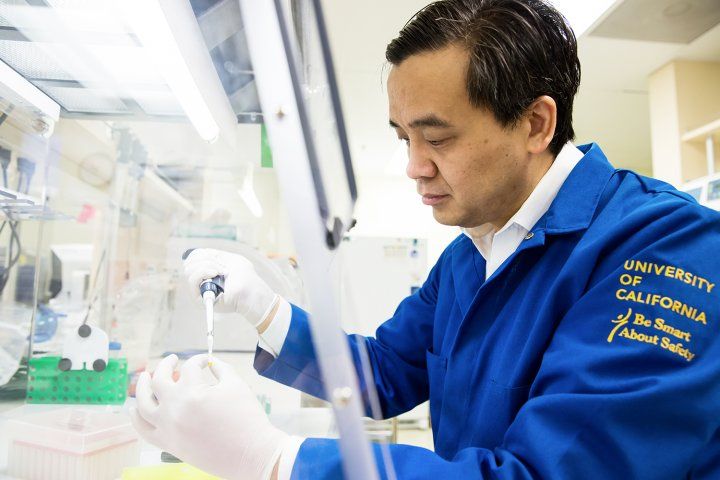
Charles Chiu, MD, PhD
The study, published June 13, 2019, in the New England Journal of Medicine, was set up to enroll only the most challenging cases. To qualify, a patient had to be hospitalized with an acute neurological illness with no conclusive diagnosis. The study included 204 pediatric and adult patients, mostly from California, who had meningitis (inflammation of the lining surrounding the brain), encephalitis (inflammation of the brain itself) or myelitis (inflammation of the spinal cord).
The test found many of the same infections identified by conventional laboratory testing methods, which generally look for pathogens one at a time, and require that doctors know what they are looking for to be successful. But it also found 13 infections that were missed by all conventional tests, such as a case of infection by St. Louis encephalitis virus, which had not been seen in California since 1986. And in more than half of those cases, the mNGS diagnosis was indispensable in guiding the treatment of these patients. In a case of hepatitis E virus infection that had been missed by conventional testing, the successful mNGS diagnosis likely spared the patient from having to undergo a liver transplant.
“The mNGS test is generally ordered as a test of last resort, and we ended up enrolling the hardest patients to diagnose,” said Chiu, also director of the UCSF-Abbott Viral Diagnostics and Discovery Center. “All conventional microbiology tests combined yield diagnoses in less than 50 percent of these patients. We’ve shown that a single test – mNGS – can make a significant dent in that number.”
In all, the test identified 32 infections of the nervous system in 31 patients. In addition to the 13 diagnoses made by mNGS only, the new technology confirmed 19 infections that had also been diagnosed by conventional tests.
Fewer than half of meningitis and encephalitis cases are caused by infections. Most of the rest are the result of autoimmune reactions, in which the patient’s own body attacks the nervous system. The two conditions require very different treatments, however – suppressing immunity in a patient with an infection can be harmful, and giving antibiotics in a case of autoimmune disease is ineffective and may unnecessarily promote antimicrobial resistance – so the first thing a doctor needs to know when treating such patients is which category of inflammatory disease they have.
“Patients with infectious and non-infectious encephalitis can be clinically indistinguishable from one another,” said Michael Wilson, MD, associate professor of neurology at UCSF, a member of the UCSF Weill Institute for Neurosciences, and co-first author of the paper, along with study coordinator Hannah Sample. “Having a broad-based test that either rules in infection or rules out infection can really aid these cases that are in gray areas between infection and not.”
The new test is not perfect, however, and there were 26 infections it could not diagnose. In the majority of these cases, DNA from the pathogen was not present in the spinal fluid, requiring analysis of a different sample type, such as tissue from a brain abscess, or use of an indirect testing method, such as antibody testing, to make the diagnosis. An example in the study was West Nile virus infection, which often cannot be identified by sequencing viral genetic material found in spinal fluid because it comes and goes so quickly.
In some cases, mNGS found hints of infections like tuberculosis that leave behind few traces in spinal fluid. But even though these infections were not detected at high enough levels to report definitively, knowing that they are present, even in trace amounts, could still aid physicians by directing them to order another diagnostic test to confirm whether the pathogen was present.
Authors: In addition to Chiu, Wilson, and Sample, authors of the new paper are Kelsey C. Zorn, Shaun Arevalo, Guixia Yu, John Neuhaus, PhD, Scot Federman, Doug Stryke , Benjamin Briggs, MD, PhD, Chaz Langelier, MD, PhD, Amy Berger, MD, PhD, Vanja Douglas, MD, S. Andrew Josephson, MD, Felicia C. Chow, MD, Brent D. Fulton, PhD, Joseph L. DeRisi, PhD, Jeffrey M. Gelfand, MD, Samia N. Naccache, PhD, Jeffrey Bender, MD, Jennifer Dien Bard, PhD, Jamie Murkey, Magrit Carlson, MD, Paul M. Vespa, MD, Tara Vijayan, MD, Paul R. Allyn, MD, Shelley Campeau, PhD, Romney M. Humphries, PhD, Jeffrey D. Klausner, MD, Czarina D. Ganzon, MD, Fatemeh Memar, Nicolle A. Ocampo, Lara L. Zimmermann, MD, Stuart H. Cohen, MD, Christopher R. Polage, MD, Roberta L. DeBiasi, MD, Barbara Haller, MD, Ronald Dallas, PhD, Gabriela Maron, MD, Randall Hayden, MD, Kevin Messacar, MD, Samuel R. Dominguez, MD, PhD, and Steve Miller, MD, PhD.
Funding: This work is supported by the California Initiative to Advance Precision Medicine, NIH grants R01HL105704, K08NS096117, K23AI28069, a UC Center for Accelerated Innovation grant funded by NIH grant U54HL119893 and NIH/NCATS UCSF-CTSI grant UL1TR000004, the Chan Zuckerberg Biohub, the Charles and Helen Schwab Foundation, the George and Judy Marcus Innovation Fund, an endowment from the Rachleff family, and the Sandler and William K. Bowes, Jr. Foundations.
Disclosures: As director of the UCSF-Abbott Viral Diagnostics and Discovery Center, Chiu receives research support from Abbott Laboratories, Inc. He is an inventor, with several other authors, on a patent application on algorithms related to software that analyzes mNGS data (SURPI+) titled “Pathogen Detection using Next-Generation Sequencing” (PCT/US/16/52912).
UC San Francisco (UCSF) is a leading university dedicated to promoting health worldwide through advanced biomedical research, graduate-level education in the life sciences and health professions, and excellence in patient care. It includes top-ranked graduate schools of dentistry, medicine, nursing and pharmacy; a graduate division with nationally renowned programs in basic, biomedical, translational and population sciences; and a preeminent biomedical research enterprise. It also includes UCSF Health, which comprises three top-ranked hospitals – UCSF Medical Center and UCSF Benioff Children’s Hospitals in San Francisco and Oakland – as well as Langley Porter Psychiatric Hospital and Clinics, UCSF Benioff Children’s Physicians and the UCSF Faculty Practice. UCSF Health has affiliations with hospitals and health organizations throughout the Bay Area. UCSF faculty also provide all physician care at the public Zuckerberg San Francisco General Hospital and Trauma Center, and the SF VA Medical Center. The UCSF Fresno Medical Education Program is a major branch of the University of California, San Francisco’s School of Medicine.