Seeking Immunity Against COVID-19
What will it take to produce a vaccine?

Immunology and infectious disease expert Joel Ernst, MD, addresses key questions about how vaccine development works and why vaccines are especially important in the case of COVID-19.

Joel Ernst, MD,
Chief of the Division of Experimental Medicine
Why are COVID-19 vaccines needed so badly?
First, this disease is highly transmissible. It’s transmitted by the respiratory route, so people spread it easily in crowded places. Obviously, it’s incapacitating and deadly. Finally, effective vaccines are the most economical means to control a transmissible infectious disease.
Another reason that vaccines have a particularly special role is that this disease can be transmitted by asymptomatic and presymptomatic individuals. In other words, somebody doesn’t have to have a fever or be coughing in order to infect the people around them.
Without a vaccine and without broad immunity in a population, COVID-19 could very well become an endemic infection. That means it remains steady in the population, like chicken pox, and unlike other pathogens that cause outbreaks and then recede, such as Ebola or Zika.
Finally, as we’re experiencing, the economic and human impacts of COVID-19 are huge.
If enough people get the virus and recover, will we achieve so-called herd immunity?
That’s pretty unlikely. There would be a lot of lives lost before we achieved a percentage of immune people in the population sufficient to prevent community transmission. In so-called herd immunity, if a high proportion (70% to 95%) of the population is immune, then a person with the disease is unlikely to cause an outbreak. To achieve that level of immunity to COVID-19 in a community through natural infection, it would mean that nearly everyone in the community would need to be infected, and with a 1% mortality rate for COVID-19, that’s unacceptable.
What do we know about immunity so far?
Part of what we know – or what we think we know – is derived from the experience with SARS, which is the most closely related coronavirus to SARS-CoV-2, the virus that causes COVID-19.
It would probably be safe to extrapolate a few things from SARS.
The first is that the protective immunity that results from infection may be transient. In people who were infected with the first SARS coronavirus, their protective immunity began waning between one and two years postinfection, as indicated by repeated checking of their antibody levels. Unlike diseases like measles or smallpox, where infection confers lifelong protective immunity, coronavirus infections may not confer long-lasting immunity.
The second thing we think we know is that neutralizing antibodies are likely to contribute to protection.
What are neutralizing antibodies? Can you talk more about antibodies in general?
When we get an infection, our immune systems respond to fight off – that is, neutralize – that specific invading virus or bacteria. These responses generally protect us against future infections from the same pathogen, unless the pathogen mutates to avoid recognition by those immune responses.

Illustrations: DrAfter123
One of the immune responses that can provide protection is the production of antibodies, proteins that recognize an infectious pathogen, with the goal of eliminating the infection. Antibodies are generally easy to measure, but the presence of antibodies does not guarantee protection. That is because the routine tests we have don’t measure the quantity or quality of antibodies.
By quality, I mean that some antibodies bind to the pathogen, but they don’t contribute to protection. They can be there, they can be detected, but they don’t possess the activities needed to eliminate the pathogen. For example, people infected with HIV generate antibodies to HIV proteins, but the HIV infection still persists.
At the extreme end, some antibodies can actually be harmful. For example, in the case of another viral disease, dengue, which is transmitted by mosquitoes, people can have antibodies that make the infection more severe and the symptoms more critical.
What all this means is: The right antibodies are needed. That’s the goal of vaccination – to confer immunity that is superior to what is conferred by infection itself.
How does a vaccine do that?
Multiple approaches to developing a COVID-19 vaccine are underway. Some are based on inactivating the virus, essentially making it noninfectious while preserving its ability to provoke an immune response; other approaches modify the virus so it can grow but not cause severe disease. Another alternative is to use a purified pathogen protein to stimulate the immune system to provoke immune responses that block the disease – an approach that’s been successful with tetanus, diphtheria, and hepatitis B vaccines.
Finally, some approaches use more advanced techniques. They work at the genetic level, embedding instructions in DNA or RNA, or they use benign viruses, called viral vectors, to deliver an antigen – the pathogen protein that induces a protective immune response – directly to cells in our immune system.
What other considerations are involved in developing a vaccine?
The goals of vaccine development are first of all, safety, and second, to induce the kind of immune response that is necessary to prevent infection and disease due to the specific pathogen; distinct pathogens can require different mechanisms to provide protective immunity.
And especially in a pandemic, rapid, large-scale production is absolutely essential. We need billions of doses of any COVID-19 vaccine. For the same reason, we need them to be economical on a global scale.
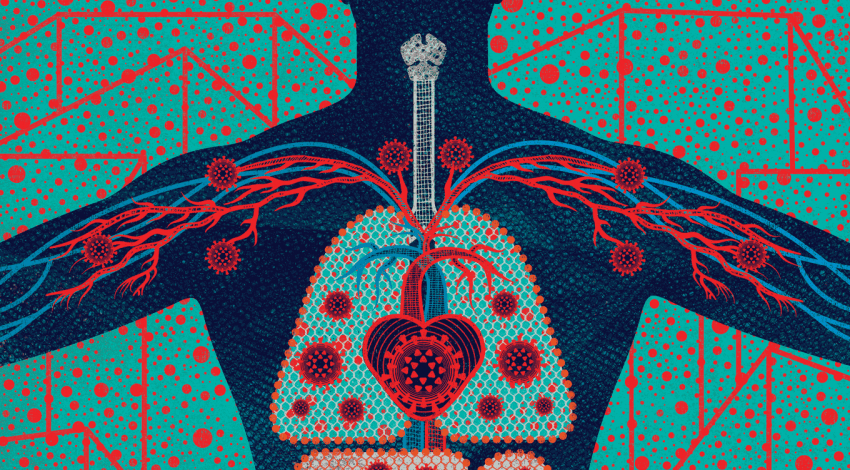
Another goal, especially in the case of COVID-19, is a vaccine that blocks the infection where the virus enters the body. Since we know that SARS-CoV-2 ordinarily enters through the respiratory tract, via the mouth or nose, we want immunity that operates right there at the portal of entry and not just in the bloodstream.
Vaccines need to generate long-lived immunological memory. Ideally, vaccines will induce immune responses that recognize viral targets that can’t mutate to escape, like the flu virus does, which forces us to modify the flu vaccine every year.
Finally, vaccines need to be stable enough for distribution to clinics worldwide. In other words, a vaccine that requires refrigeration is not going to reach everyone.
What vaccine development activity is underway right now?
There are at least 90 groups worldwide working to develop COVID-19 vaccines. Roughly 20 of them are working on DNA- or RNA-based vaccines, about 25 groups are working on viral-vector vaccines, and numerous groups are working on protein-based vaccines. A smaller number of groups are working on viruslike protein particles, which are a bit more difficult and expensive to produce. Here at UCSF, there are many experts in immunology and virology working to assure that new COVID-19 vaccines have the properties that are most important.
To have a global impact, a vaccine needs to work in large, diverse populations. And those steps can only be combined or rushed to a limited extent.”
What comes after discovery and development?
The next stage is human studies. They address the question, Is the new vaccine safe? Can you give it to people without causing undue toxicity? The next question is, Does the vaccine stimulate immune responses in humans? Next, Does the vaccine protect humans from disease in a so-called efficacy trial? Finally, Does the vaccine protect humans in the real world? That is called “vaccine effectiveness.” The difference between efficacy and effectiveness is that in efficacy studies, the conditions and subjects are chosen to be ideal for the study. Effectiveness means that the vaccine protects people who aren’t preselected, who might have medical conditions that could make it more challenging for a vaccine to work. To have a global impact, a vaccine needs to work in large, diverse populations. And those steps can only be combined or rushed to a limited extent.
A recent clinical trial led by the pharmaceutical company Moderna showed promising – but very preliminary – results. Can you interpret their findings?
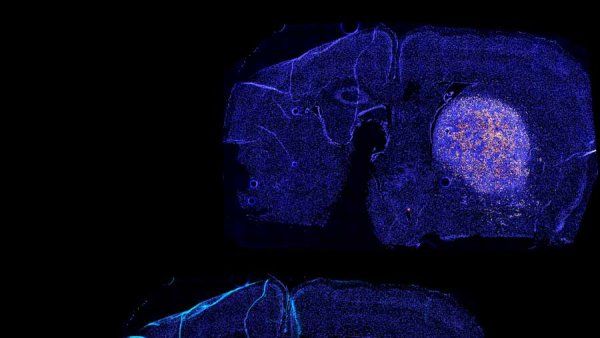
This was a safety trial of an RNA vaccine. It was designed to test how well 45 healthy volunteers tolerated different doses of the vaccine. But supplemental data showed that the volunteers produced antibodies similar to those in people who have recovered from the virus, suggesting the vaccine achieved the sought-after immune response. While finding antibodies is good news, it does not tell us if the vaccine is effective.
What happens next?
An expanded safety trial. In 45 subjects, you’re only going to see the most common side effects – things like pain at the injection site, a fever. To capture rare side effects, it’s necessary to expand the number of study participants. It would also be expanded into different groups, including older people. The upper age cutoff of these volunteers was 55 years. We know that older people are more susceptible to bad outcomes from COVID-19, so it’s important to determine whether the same vaccine at the same dose also produces an immune response in them.
How do we know whether or not a vaccine provides protection?
Through efficacy studies, which follow safety studies. Efficacy studies can be done in one of two main ways. They can be done in very large populations at risk – you vaccinate some and don’t vaccinate others and compare the rates of infection in the two groups. Those are expensive, they take a long time, and they can be complicated by fluctuations in the frequency of the disease in question. For example, if a flu vaccine trial was started after the peak of flu season, the rate of infection in both groups might be too low to find a difference in infection rates.
The other alternative is a human challenge study. In that case, people are vaccinated or not and then actually challenged with the pathogen of interest. Challenge studies are generally done with pathogens for which there’s curative therapy – malaria, for example. You watch for evidence that a person develops a fever and treat them immediately with that therapy. We don’t have that advantage in the case of the new coronavirus, since we don’t currently have a highly effective treatment.
How should we set our expectations?
I think we’re roughly 12 to 18 months from being able to roll out a vaccine that’s accessible to a significant slice of the population.